Systematic review with meta-analysis of transverse vs. vertical midline extraction incisional hernia risk following laparoscopic colorectal resections
Highlight box
Key findings
• Transverse incision for specimen extraction following laparoscopic colorectal resection seems to have of incisional hernia compared to midline incision.
What is known and what is new?
• Incisional hernia is evidenced to be one of the most common complications following laparoscopic colorectal resections; hence several actions has been adapted to reduce the incidence naming, using off-midline approach, small bites and prophylactic mesh. An off-midline approach has been shown to be effective in reducing the risk of incisional hernia in many comparative trials. The finding of current meta-analysis of 25 comparative studies (including two RCTs) on a sample size of 10,362 is consistent with the outcomes of previously published meta-analysis.
What is the implication, and what should change now?
• Furthermore, studies need to be done to compare the different type of closing materials (sutures/mesh) and techniques in order to find the best method of reducing incisional hernia incidence.
Introduction
In recent years, laparoscopic surgery is considered standard for most of the colorectal pathology including malignancy. Even in laparoscopic approach, a mini laparotomy is often done for specimen extraction (1,2). Having an incidence of 3% to 20% (3), incisional hernia is considered a common complication. European Hernia Society Guidelines define incisional hernia as any abdominal wall gap with or without a bulge in the area of a postoperative scar perceptible or palpable by clinical examination or imaging (4). Almost half of the incidences are picked up within the first year following surgery although they can occur afterwards (5). More than one third of incisional hernia patients complain of pain, discomfort, bowel obstruction, restricted mobility and overall delayed recovery (6). There is evidence that suggests these patients reporting low score for physical and social functioning and overall general health perception (7) About 17% patients present with strangulated/incarcerated hernia requiring emergency surgery (8). In the United States, approximately 360,000 incisional hernia repairs are done per year with a total estimated cost of 3.2 billion USD per year (9). There is existing evidence and recommendations on the use of transverse and off-midline approach for mini laparotomy showing a reduced incidence of incisional hernia (10,11). Some high-quality trials have also showed the effectiveness of enhanced closure techniques, such as small bites and prophylactic mesh (12,13). Aim of the present study is to perform a systematic review and meta-analysis to compare the incidence of incisional hernia at the extraction site with a primary emphasis on the location of the incision, comparing between transverse incision and midline vertical incision. We present the following article in accordance with PRISMA reporting checklist (available at https://tgh.amegroups.com/article/view/10.21037/tgh-22-75/rc).
Methods
Data sources and literature search technique
Literature search was thoroughly carried out from electronic databases like MEDLINE, EMBASE, PubMed and Cochrane Library using the MeSH search terms. Boolean operators (AND, OR, NOT) were used for extended search result. The titles were carefully looked at for study selection. Moreover, references from curated articles were examined to find additional relevant trials
Trial selection
The primary inclusion criteria for the meta-analysis were the comparison of the risk of incisional hernia at the specimen extraction site following laparoscopic colorectal resection, emphasising mainly on transverse incision versus midline vertical abdominal incision.
Data collection and management
Reported data were collected from the included trials by independent reviewers on a standard data extraction form. The collected dataset was matched and found to be in satisfactory inter-reviewer agreement. The extracted data consisted of list of the authors, title of the published study, journal of publication, country and year of the publication, testing sample size (with gender differentiation if applicable), the number of patients in each group based on the incision type and site, treatment protocol for each intervention, and duration of follow up. Following data extraction, the reviewers went through discussing their respective results and a consensus of mutual agreement was reached in likely discrepancies.
Statistical analysis
Statistical analysis was performed using RevMan 5.3 (Review manager 5.3, The Nordic Cochrane Centre, Copenhagen, Denmark). The risk ratio (RR) and a confidence interval (CI) of 95% were used for binary data and random-effects model (14,15) was used for both binary and continuous variables. Heterogeneity was calculated by inspecting the forest plots and by computing the chi2 test, with significance set at P<0.05 as well as using I2 test with a maximum value of 30 per cent identifying low heterogeneity (16). The Mantel-Haenszel method was used for the calculation of RR under the random effect model (17) analysis. In a sensitivity analysis, 0.5 was added to each cell frequency for trials in which no event occurred in either the treatment or control group, according to the method recommended by Deeks et al. (18). If the standard deviation was not available, then the risk of bias was calculated according to the guidelines provide by the Cochrane Collaboration (14). This process assumed that both groups had the same variance, which may not have been true, and variance was either estimated from the range or from the p-value. The estimate of the difference between both techniques was pooled, depending upon the effect weights in results determined by each trial estimate variance. A forest plot was used for the graphical display of the results. The square around the estimate stood for the accuracy of the estimation (sample size), and the horizontal line represented the 95% CI. The methodological quality of the included trials was initially assessed using the published guidelines of Jadad et al., Chalmers et al. and Rangel et al. (19-21).
Endpoint
Post-operative occurrence of extraction site incisional hernia comparing vertical midline and transverse incision was assessed as the primary endpoint in this meta-analysis.
Results
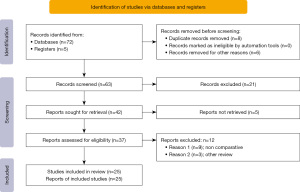
The initial database search generated 63 studies after removing 14 duplicate studies. After initial title and abstract assessment 21 studies were excluded. Forty-two studies were sought for retrieval, 5 were not found. Finally 37 studies were assessed for inclusion and 25 were found to be appropriate according to the inclusion criteria (Figure 1).
Characteristics and demographics of included studies
Eighteen retrospective trials (22-39), five prospective studies (40-44) and two RCTs (45,46) on 10,362 patients were included to conduct this meta-analysis based upon the principles provide by the Cochrane Collaboration. The PRISMA flow chart for trial selection is given in Figure 1. The included trials were conducted in USA (22,23,27,30,35,36,41,44,46), Italy (24), Spain (25,40), Korea (26,31,34,43), Japan (28,37), Canada (32,33,45), Israel (29,42), Australia (38) and UK (38,39). The number of patients who were involved varies between the trials ranging between 33 (44) to 2,704 (26). All the trials were conducted between 2000 (23) and 2019 (26). Four studies (27,29,30,33) reported a range of 10–19 months as the duration of follow-up. Nine studies (25,32,34,35,36,37,38,44,45) fall in the range of 20–29 months, 30–39 months in four studies (31,42,43,46), 40–49 months in six studies (24,26,28,32,39,41) were reported as the duration of follow-up. In the remaining trials (22,23), the follow-up period was more than 50 months, the highest reported being 72 months (23). The mean age of patient included in the trial was ranging from 38.9 (35) to 75.15 (39). There was no discrimination for study selection in terms of gender, age, number of recruited patients and language of the published study. Main characteristics of the included studies are given in Table 1 and the treatment protocol adopted in each of the study is given in Table 2.
Table 1
| Title | Year | Country | Study design | Total patient | IH | Age (years) | Male: female | Follow up (months) | Duration |
|---|---|---|---|---|---|---|---|---|---|
| Aquina (22) (vertical; transverse) | 2015 | USA | Retrospective | 193 | 8; 3 | 66.4 | 1.16:1 | 56.4 | 2003–2010 |
| Benlice (23) (vertical; transverse) | 2016 | USA | Retrospective | 2,148 | 35; 11 | 57.5±16.6; 46.7±16.9 | 7:10.5; 2.4:1 | 72.5±41.8; 60.8±28.6 | 2000–2011 |
| Campagnacci (24) (vertical; transverse) | 2015 | Italy | Retrospective | 748 | 45; 3 | 64.9; 66 | Not included | 48 | 2004–2012 |
| Cano-Valderrama (25) (vertical; transverse) | 2020 | Spain | Retrospective | 225 | 34; 5 | 68.7 | 1.1:1 | 28.8 | 2014–2016 |
| Choi (26) (vertical; transverse) | 2022 | Korea | Retrospective | 2,704 | 52; 21 | 68.5±9.6 | 1:1.1 | 41 | 2006–2019 |
| DeSouza (27) (vertical; transverse) | 2011 | USA | Retrospective | 512 | 65; 0 | 62.68; 61.32 | 1:1.3; 1:1.1 | 18.49; 17.53 | 2004–2007 |
| Fukuoka (28) (vertical; transverse) | 2021 | Japan | Retrospective | 423 | 36; 0 | 72 | 1:1.1; 1 | 48.4 | 2012–2014 |
| Greemland (29) (vertical; transverse) | 2021 | Israel | Retrospective | 138 | 42; 12 | 71.40±8.87 | 1:1.7 | 15.3 | 2011–2016 |
| Harr (30) (vertical; transverse) | 2016 | USA | Retrospective | 259 | 14; 1 | 61.5±13.8; 57.5±12.4 | 1.09:1; 1:1.7 | 17.25±15.21 | 2009–2014 |
| Lee (31) (vertical; transverse) | 2012 | Canada | Retrospective | 99 | 20; 1 | 63; 65.8 | 13:8; 3:4 | 28.3; 44.1 | 2003–2009 |
| LaChapelle (32) (vertical; transverse) | 2020 | USA | Retrospective | 423 | 1; 0 | 43.8; 38.9 | 1.5:1; 1:1.2 | 21.9; 22.2 | 2008–2016 |
| Llaguna (33) (vertical; transverse) | 2010 | USA | Retrospective | 218 | 26; 4 | 64.2±13.3 | 12:5 | 24.2±10.6 | 2002–2007 |
| Morita (34) (vertical; transverse) | 2015 | Japan | Retrospective | 206 | 1; 6 | 65.0±10.4; 64.5±10.3 | 29:18; 15:8 | 24 | 2008–2011 |
| Navaratnam (35) (vertical; transverse) | 2015 | UK; Australia | Retrospective | 224 | 5; 13 | 68.8; 65.4 | 72:67; 41:44 | 24 | 2005–2009 |
| Pereira (36) (vertical; transverse) | 2019 | Spain | Retrospective | 182 | 23; 16 | 70.4; 68.8 | 1.5:1; 1.35:1 | 13 | 2015–2016 |
| Samia (37) (vertical; transverse) | 2013 | USA | Retrospective | 480 | 27; 5 | 65.1±13.5 | 19:13 | 45.9±15.6 | 2005–2012 |
| Shapiro (38) (vertical; transverse) | 2016 | Israel | Retrospective | 191 | 17; 0 | 72 | 1:1.2 | 33.7 | 2006–2014 |
| Sadava (39) (vertical; transverse) | 2016 | USA | Retrospective | 33 | 4; 4 | 60 | 2:1 | 20 | 2001–2014 |
| Ku (40) (vertical; transverse) | 2020 | Korea | Prospective | 189 | 22; 23 | 64.3±11.2; 64.9±10.7 | 1.6:1; 2:1 | 31 | 2010–2017 |
| Lim (41) (vertical; transverse) | 2013 | Korea | Prospective | 147 | 2; 0 | 63; 66 | 61:31; 37:18 | 20.0±5.4 | 2010 |
| Parés (42) (vertical; transverse) | 2016 | UK | Prospective | 292 | 16; 4 | 75.15±6.9 | 2:3 | 42 | 2006–2013 |
| Shin (43) (vertical; transverse) | 2016 | Korea | Prospective | 114 | 1; 2 | 65.0 | 37:20; 39:18 | 31 | 2010–2014 |
| Singh (44) (vertical; transverse) | 2008 | Canada | Prospective | 166 | 13; 0 | 64.0±13.4 | 7:8 | 20.2±14.4 | 2002–2006 |
| Lee (45) (vertical; transverse) | 2018 | Canada | RCT | 141 | 6; 1 | 66.4±12.1; 66.6±12.4 | 1.08:1; 1.2:1 | 12 | 2011–2016 |
| Tan (46) (vertical; transverse) | 2015 | USA | RCT | 40 | 1; 0 | 57; 61.5 | 1:1; 13:7 | 30 | 2010–2011 |
IH, incisional hernia; RCT, randomized controlled trial.
Table 2
| Title | Midline vertical incision closure technique | Transverse incision closure technique |
|---|---|---|
| Aquina (22) | NR | NR |
| Benlice (23) | Mass closure running; 0- polydioxanone | Full thickness; running; 1 polyglactin |
| Campagnacci (24) | Interrupted; 2-0 glycolide/lactide co-polymer | Interrupted; 2-0 glycolide/lactide co-polymer |
| Cano-Valderrama (25) | Running; polyglactin 910 or polydioxanone | Running; polyglactin 910 or polydioxanone |
| Choi (26) | NR | NR |
| DeSouza (27) | Continuous polydioxanone | Continuous polydioxanone |
| Fukuoka (28) | Interrupted 1 vicryl for fascia and 4-0 PDS for skin (subcuticular) | Interrupted 1 vicryl for fascia and 4-0 PDS for skin(subcuticular) |
| Greemland (29) | Loop polydioxanone suture, nylon “0” in 1 layer, or interrupted absorbable verticalcryl “0” sutures | Loop polydioxanone suture, nylon “0” in 1 layer, or interrupted absorbable verticalcryl “0” sutures |
| Harr (30) | Running, 0- polydioxanone | Running, 0- polydioxanone |
| Lee (31) | Single layer continuous. 1 polydioxanone | Two layers continuous 1 polydioxanone |
| LaChapelle (32) | NR | NR |
| Llaguna (33) | #1 polydioxanone (PDS) for fascia and skin clips | #1 polydioxanone (PDS) for fascia and skin clips |
| Morita (34) | Single layer, absorbable | Single layer, oblique muscle suture |
| Navaratnam (35) | NR | NR |
| Pereira (36) | Interrupted 1-0 polyglactin | Continuous 3/0 polyglactin |
| Samia (37) | NR | NR |
| Shapiro (38) | NR | NR |
| Sadava (39) | No. 1 polyglactin | No. 1 polyglactin |
| Ku (40) | Single layer, interrupted polyglactin | Single layer, interrupted polyglactin |
| Lim (41) | Single layer; 1 polyglactin | Two layers; 1 polyglactin |
| Parés (42) | Single layer, Continuous, 1-polydioxanone | Two layers; continuous, 1 polydioxanone |
| Shin (43) | NR | NR |
| Singh (44) | Single layer, 1 Verticalcryl | Two layers ,1 verticalcryl |
| Lee (45) | Continuous 1–0 polydioxanone | Two layers; continuous 1–0 polydioxanone |
| Tan (46) | Looped 1 polydioxanone | Looped 1 polydioxanone |
NR, not reported.
Methodological quality of included studies
The methodological quality of included trials is summarized in Table 3. The Mantel-Haenszel random effects model was used to compute robustness and susceptibility to any outlier among these trials. The randomization in randomized trials was done using computer generated random numbers, and the concealment was done using sealed envelopes (33,46). However, the blinding was not adopted in either randomized trial. The quality of the 23 comparative studies (retrospective & prospective) were analysed by using the Scottish Intercollegiate Guidelines Network and Dudgeon et al. (21), and eight studies were found to have good quality (26,29,31,32,34,35,39,43), and the rest were of fair quality.
Table 3
Outcome of the primary variable
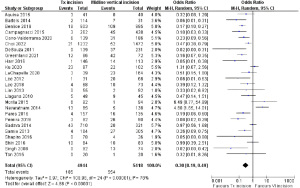
In the analysis, the use of transverse incision for specimen extraction is found to have less the risk of IH development (odds ratio =0.30, 95% CI: 0.19–0.49, Z=4.88, P=0.00001). However, there was significant heterogeneity (Tau2=0.97; χ2=109.98, df=24, P=0.00004; I2=78%) among included studies (Figure 2).
Discussion
Incisional hernia is evidenced to be one of the most common complications following laparoscopic colorectal resections; hence several actions has been adapted to reduce the incidence naming, using off-midline approach, small bites and prophylactic mesh. An off-midline approach has been shown to be effective in reducing the risk of incisional hernia in many comparative trials. The outcome of this study comparing 25 trials on a sample size of 10,362 is consistent with the outcome of previously published meta-analysis (47). The previous meta-analysis analysed fewer number of trials with fewer number of patients (47). To the best of our knowledge this is the only meta-analysis on the highest number [10,362] of patients reporting the effectiveness of using off-midline incision especially transverse to reduce the risk of extraction site incisional hernia. Also, all the comparative studies included are of fair to good quality well according to the criteria of quality assessment. Thus, it provides a relatively stronger evidence to consider routine use of transverse incision in patients undergoing laparoscopic colorectal resections. There are a number of limitations in this study. Due to lack of RCTs, this study includes both prospective and retrospective studies along with 2 RCTs which makes the meta-analysis potentially biased in source of evidence. A number of multicentre larger RCTs are required to support this study before making regular recommendations of using transverse incision. Furthermore, studies need to be done to compare the different type of closing materials (sutures/mesh) and techniques in order to find the best method of reducing incisional hernia incidence at specimen extraction site following laparoscopic colorectal resection.
Conclusions
Transverse incision used for specimen extraction seems to reduce the risk of postoperative IH incidence compared to vertical midline abdominal incisions based on our meta-analysis.
Acknowledgments
The abstract of this article has been published in British Journal of Surgery, Volume 109, August 2022.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://tgh.amegroups.com/article/view/10.21037/tgh-22-75/rc
Peer Review File: Available at https://tgh.amegroups.com/article/view/10.21037/tgh-22-75/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tgh.amegroups.com/article/view/10.21037/tgh-22-75/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Clinical Outcomes of Surgical Therapy Study Group. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 2004;350:2050-9. [Crossref] [PubMed]
- Laurent C, Leblanc F, Bretagnol F, et al. Long-term wound advantages of the laparoscopic approach in rectal cancer. Br J Surg 2008;95:903-8. [Crossref] [PubMed]
- Sanders DL, Kingsnorth AN. The modern management of incisional hernias. BMJ 2012;344:e2843. [Crossref] [PubMed]
- Muysoms FE, Miserez M, Berrevoet F, et al. Classification of primary and incisional abdominal wall hernias. Hernia 2009;13:407-14. [Crossref] [PubMed]
- Mudge M, Hughes LE. Incisional hernia: a 10 year prospective study of incidence and attitudes. Br J Surg 1985;72:70-1. [Crossref] [PubMed]
- Bucknall TE, Cox PJ, Ellis H. Burst abdomen and incisional hernia: a prospective study of 1129 major laparotomies. Br Med J (Clin Res Ed) 1982;284:931-3. [Crossref] [PubMed]
- van Ramshorst GH, Eker HH, Hop WC, et al. Impact of incisional hernia on health-related quality of life and body image: a prospective cohort study. Am J Surg 2012;204:144-50. [Crossref] [PubMed]
- Read RC, Yoder G. Recent trends in the management of incisional herniation. Arch Surg 1989;124:485-8. [Crossref] [PubMed]
- Poulose BK, Shelton J, Phillips S, et al. Epidemiology and cost of ventral hernia repair: making the case for hernia research. Hernia 2012;16:179-83. [Crossref] [PubMed]
- Brown SR, Goodfellow PB. Transverse verses midline incisions for abdominal surgery. Cochrane Database Syst Rev 2005;2005:CD005199. [PubMed]
- Muysoms FE, Antoniou SA, Bury K, et al. European Hernia Society guidelines on the closure of abdominal wall incisions. Hernia 2015;19:1-24. [Crossref] [PubMed]
- Deerenberg EB, Harlaar JJ, Steyerberg EW, et al. Small bites versus large bites for closure of abdominal midline incisions (STITCH): a double-blind, multicentre, randomised controlled trial. Lancet 2015;386:1254-60. [Crossref] [PubMed]
- Jairam AP, Timmermans L, Eker HH, et al. Prevention of incisional hernia with prophylactic onlay and sublay mesh reinforcement versus primary suture only in midline laparotomies (PRIMA): 2-year follow-up of a multicentre, double-blind, randomised controlled trial. Lancet 2017;390:567-76. Erratum in: Lancet 2017;390:554. [Crossref] [PubMed]
- DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177-88. [Crossref] [PubMed]
- Demets DL. Methods for combining randomized clinical trials: strengths and limitations. Stat Med 1987;6:341-50. [Crossref] [PubMed]
- Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539-58. [Crossref] [PubMed]
- Matthias E, Davey SG, Altman DG. editors. Systematic reviews in health care: meta-analysis in context. 2nd edition. London: BMJ Publishing Group, 2001; 487.
- Deeks JJ, Altman DG, Bradburn MJ. Statistical Methods for Examining Heterogeneity and Combining Results from Several Studies in Meta-Analysis. In: Egger M, Smith GD, Altman DG. editors. Systematic Reviews in Health Care: Meta-Analysis in Context. 2nd ed. Londong: John Wiley & Sons, Ltd, 2001: 285-312.
- Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996;17:1-12. [Crossref] [PubMed]
- Chalmers TC, Smith H Jr, Blackburn B, et al. A method for assessing the quality of a randomized control trial. Control Clin Trials 1981;2:31-49. [Crossref] [PubMed]
- Dudgeon D, Rangel S. Development of a quality assessment scale for retrospective clinical studies in paediatric surgery. J Pediatr Surg 2003;38:396.
- Aquina CT, Rickles AS, Probst CP, et al. Visceral obesity, not elevated BMI, is strongly associated with incisional hernia after colorectal surgery. Dis Colon Rectum 2015;58:220-7. [Crossref] [PubMed]
- Benlice C, Stocchi L, Costedio MM, et al. Impact of the Specific Extraction-Site Location on the Risk of Incisional Hernia After Laparoscopic Colorectal Resection. Dis Colon Rectum 2016;59:743-50. [Crossref] [PubMed]
- Campagnacci R, Baldoni A, Ghiselli R, et al. Prevention of hernia incision in laparoscopic left colon resection. Minerva Chir 2015;70:155-60. [PubMed]
- Cano-Valderrama O, Sanz-López R, Domínguez-Serrano I, et al. Extraction-site incisional hernia after laparoscopic colorectal surgery: should we carry out a study about prophylactic mesh closure? Surg Endosc 2020;34:4048-52. [Crossref] [PubMed]
- Choi HB, Chung D, Kim JS, et al. Midline incision vs. transverse incision for specimen extraction is not a significant risk factor for developing incisional hernia after minimally invasive colorectal surgery: multivariable analysis of a large cohort from a single tertiary center in Korea. Surg Endosc 2022;36:1199-205. [Crossref] [PubMed]
- DeSouza A, Domajnko B, Park J, et al. Incisional hernia, midline versus low transverse incision: what is the ideal incision for specimen extraction and hand-assisted laparoscopy? Surg Endosc 2011;25:1031-6. [Crossref] [PubMed]
- Fukuoka H, Watanabe J, Masanori O, et al. The risk factors for incisional hernia after laparoscopic colorectal surgery: a multicenter retrospective study at Yokohama Clinical Oncology Group. Surg Endosc 2021;35:3471-8. [Crossref] [PubMed]
- Greemland I, Raveh G, Gavrielli S, et al. High Rates of Incisional Hernia After Laparoscopic Right Colectomy With Midline Extraction Site. Surg Laparosc Endosc Percutan Tech 2021;31:722-8. [Crossref] [PubMed]
- Harr JN, Juo YY, Luka S, et al. Incisional and port-site hernias following robotic colorectal surgery. Surg Endosc 2016;30:3505-10. [Crossref] [PubMed]
- Lee L, Mappin-Kasirer B, Sender Liberman A, et al. High incidence of symptomatic incisional hernia after midline extraction in laparoscopic colon resection. Surg Endosc 2012;26:3180-5. [Crossref] [PubMed]
- LaChapelle CR, Whitney S, Aalberg J, et al. Analysis of Outcomes by Extraction Site following Subtotal Colectomy in Ulcerative Colitis: A Retrospective Cohort Study. J Gastrointest Surg 2020;24:933-8. [Crossref] [PubMed]
- Llaguna OH, Avgerinos DV, Lugo JZ, et al. Incidence and risk factors for the development of incisional hernia following elective laparoscopic versus open colon resections. Am J Surg 2010;200:265-9. [Crossref] [PubMed]
- Morita Y, Yamaguchi S, Ishii T, et al. Does transumbilical incision increase incisional hernia at the extraction site of laparoscopic anterior resection? Am J Surg 2015;209:1048-52. [Crossref] [PubMed]
- Navaratnam AV, Ariyaratnam R, Smart NJ, et al. Incisional hernia rate after laparoscopic colorectal resection is reduced with standardisation of specimen extraction. Ann R Coll Surg Engl 2015;97:17-21. [Crossref] [PubMed]
- Pereira JA, Pera M, López-Cano M, et al. Hernias at the extraction incision after laparoscopic colon and rectal resection: Influence of incision location and use of prophylactic mesh. Cir Esp 2019;97:20-6. (Engl Ed). [Crossref] [PubMed]
- Samia H, Lawrence J, Nobel T, et al. Extraction site location and incisional hernias after laparoscopic colorectal surgery: should we be avoiding the midline? Am J Surg 2013;205:264-7; discussion 268. [Crossref] [PubMed]
- Shapiro R, Keler U, Segev L, et al. Laparoscopic right hemicolectomy with intracorporeal anastomosis: short- and long-term benefits in comparison with extracorporeal anastomosis. Surg Endosc 2016;30:3823-9. [Crossref] [PubMed]
- Sadava EE, Schlottmann F, Bun ME, et al. Laparoscopic incisional hernia repair after colorectal surgery. Is it possible to maintain a mini-invasive approach? Surg Endosc 2016;30:5290-4. [Crossref] [PubMed]
- Ku DH, Kim HS, Shin JY. Short-term and Medium-term Outcomes of Low Midline and Low Transverse Incisions in Laparoscopic Rectal Cancer Surgery. Ann Coloproctol 2020;36:304-10. [Crossref] [PubMed]
- Lim SW, Huh JW, Kim YJ, et al. Vertical transumbilical incision versus left lower transverse incision for specimen retrieval during laparoscopic colorectal surgery. Tech Coloproctol 2013;17:59-65. [Crossref] [PubMed]
- Parés D, Shamali A, Stefan S, et al. Predictive factors for extraction site hernia after laparoscopic right colectomy. Int J Colorectal Dis 2016;31:1323-8. [Crossref] [PubMed]
- Shin JY. Right lower transverse incision versus vertical transumbilical incision for laparoscopic specimen extraction in patients with left-sided colorectal cancer: a comparative study of two mini-laparotomy techniques. World J Surg Oncol 2016;14:274. [Crossref] [PubMed]
- Singh R, Omiccioli A, Hegge S, et al. Does the extraction-site location in laparoscopic colorectal surgery have an impact on incisional hernia rates? Surg Endosc 2008;22:2596-600. [Crossref] [PubMed]
- Lee L, Mata J, Droeser RA, et al. Incisional Hernia After Midline Versus Transverse Specimen Extraction Incision: A Randomized Trial in Patients Undergoing Laparoscopic Colectomy. Ann Surg 2018;268:41-7. [Crossref] [PubMed]
- Tan WS, Chew MH, Ho KS, et al. Short and long-term outcomes of a randomised controlled trial of vertical periumbilical wound versus transverse left iliac fossa wound for specimen retrieval in laparoscopic anterior resections. Surg Endosc 2015;29:2720-7. [Crossref] [PubMed]
- Lee L, Abou-Khalil M, Liberman S, et al. Incidence of incisional hernia in the specimen extraction site for laparoscopic colorectal surgery: systematic review and meta-analysis. Surg Endosc 2017;31:5083-93. [Crossref] [PubMed]
Cite this article as: Ahsan A, Nour HM, Peristeri DV, Abogabal S, Swaminathan C, Sajid MS. Systematic review with meta-analysis of transverse vs. vertical midline extraction incisional hernia risk following laparoscopic colorectal resections. Transl Gastroenterol Hepatol 2023;8:16.