Splenic laceration after routine colonoscopy, a case report of a rare iatrogenic complication
Case presentation
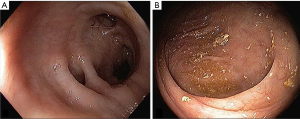
A 65-year-old Caucasian female with a history of colon polyps presented to her gastroenterologist for routine screening colonoscopy. Usual colonic preparations were followed. Findings include sigmoid diverticular disease. A 5 mm sessile polyp (pathology proven hyperplastic polyp) was removed 30 centimeter from the anal verge without initial complication (Figure 1). Immediately post procedure, the patient complained of epigastric discomfort and excessive gas. Vital signs were within normal limits. The patient’s pain improved slightly and she was discharged to home care after two hours of observation.
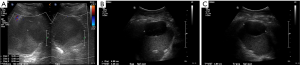
After discharge, the patient experienced persistent, severe left upper quadrant pain for two weeks, at which point the patient presented to the emergency department (ED). A prompt Computer Tomography (CT) scan of the abdomen and pelvis with intravenous and oral contrast was performed. The CT demonstrated a subcapsular hypodense collection (size 8.1×3.7×7.8 cm) in the spleen, without hemoperitoneum. A thin 1.8 cm splenic laceration was noted at the lateral aspect of the spleen (Figure 2). This was classified as a grade II splenic injury using the Organ Injury Scale from the American Association for the Surgery of Trauma (AAST). The patient remained hemodynamically stable during the ED visit. After 6 hours of observation, she was discharged with oral analgesic pain control and short-term follow-up.

An outpatient abdominal ultrasound performed 7 days after the ED visit demonstrated a slight retraction of the subcapsular hematoma (Figure 3, size 8.1×5.5×5.3 cm). Continued follow-up ultrasound 14 days after ED visit showed continued retraction of the subcapsular hematoma (Figure 3, size 6.1×4.5×5.2 cm). Given continued hemodynamic stability and decreased pain, no further imaging follow-up was obtained. To date, patient remains healthy without further complication.
Discussion
Colonoscopy is a common procedure, with a CDC survey estimating that 22.4 million colonoscopies were performed in the United States in 2004 (1). Approximately 65% of US adults undergo colonoscopy for screening and surveillance of colorectal cancer (2). The overall serious adverse event rate is estimated to be 2.8 per 1,000 procedures (3). Common serious complications include cardiopulmonary complications related to sedation, intestinal perforation, hemorrhage, post-polypectomy electrocoagulation syndrome, infection, and combustion of intestinal gases (4). Polypectomy during a colonoscopy is associated with a 7-fold increase risk of adverse events (5).
Splenic injury is a rare iatrogenic injury from colonoscopy, with reported injuries ranging from splenic laceration to capsular rupture with hemoperitoneum. According to Jehangir et al., 172 cases were reported prior to 2015 (6). Previous reports estimated an incidence rates of splenic injury ranging from 1 in 100,000 to 1 in 6,387 colonoscopies (7). Although rare, this complication is significant. A traumatic splenic injury requiring splenectomy have been reported to have a mortality rate of 25% (8). With increasing average age of the American population as baby boomers enter retirement, there will be an increasing number of colonoscopy performed. Given the estimated colonoscopy performed, this extrapolates to an annual incidence of at least 224 cases of splenic injury in the United States alone if we assume an incidence rate of 1 in 100,000. Yet, only 172 cases have been reported in the medical literature to date. This suggests the majority of splenic injuries resulting from colonoscopy may be undetected or not reported. The possible reasons for this includes misattribution of pain to gas discomfort, particularly in hemodynamically stable patients. As a case in point, our index case was detected two week post colonoscopy and would have been missed if not for the prompt investigation in the ED. Authors from previous publications also share the opinion that splenic injury from a colonoscopy is likely under-reported and under-detected (9-11).
Overall, splenic injury from colonoscopy is more prevalent in women with a near 3 to 1 ratio for unknown reasons (10).
Advanced age is proposed to be a possible risk factor for splenic injury, with average age of occurrence of 63.0 years (10). However, this may be less of a risk factor, but rather an indicator of the patient population undergoing colonoscopies. The use of anticoagulants has been reported in some of the previous cases, but does not correlate with splenic injury (12). Approximately half of the patients with splenic injury were reported to have undergone previous abdominal surgery (13). Overall, it is our opinion that no definitely conclusions regarding risk factor(s) can be drawn from the current number of cases.
The mechanisms of injury are proposed to be traction on the splenocolic ligament and/or due to adhesions between the splenic flexure and the spleen in patients with prior abdominal surgery. Other factors associated with injury includes instrument looping and presence of mass and/or polyp at the splenic flexure (14). Direct force exerted on the spleen during colonoscopy is also a possible mechanism of injury (10). Additionally, excess traction on the ligaments from external pressure during straightening of the scope on the left hypochondrium may simulate a blunt abdominal trauma (13).
Clinically, patients often present with pain after colonoscopy. Typically, the onset of pain is immediate post procedure, though, in a portion of patients, abdominal pain may be delayed for up to 24 hours after the procedure. Kehr’s sign refers to left shoulder pain upon bimanual palpation of the left upper quadrant was reported in 34% of the patients. Patients may or may not present with a drop in hematocrit and hemodynamic instability, depending on the degree of splenic injury (14). In our index case, the pain was immediate post procedure and persisted for nearly two weeks prior to diagnosis. Endoscopists and other clinical providers involved in patient care should have a high index of suspicion for splenic injury, particularly with a constellation of left upper quadrant pain and hemodynamic instability (15).
Contrast-enhanced CT is the ideal test for diagnosis of splenic trauma (16). This modality is readily available in most hospital settings and allows for rapid diagnosis and grading of splenic injury. Furthermore, CT can evaluate for other possible complications from colonoscopy that have similar clinical presentations, including perforation or infection. The Organ Injury Scale from the American Association for Surgeries of Trauma (AAST) is often used to classify the degree of splenic trauma as seen on http://www.aast.org (17). A contrast blush, if seen during CT can be predictive of non-operative management failures (18). Ultrasound is a helpful adjunct method of evaluation; this modality can visualize free fluid within the abdomen and potential hematoma adjacent the spleen. A Focused Assessment with Sonography for Trauma (FAST) is used in the emergent setting as FAST is easily performed at the bedside, and able to provide a rapid diagnosis of intra-abdominal fluid (19). A plain radiograph is of limited utility, as it does not allow for easy evaluation of the spleen, and would only yield a positive result in cases associated with hollow organ perforation.
Treatment depends on the severity of the splenic injury. Patients with normal blood pressure and hematocrit, a lower grade of splenic injury and low quantity of hemoperitoneum perform better with conservative non-operative/non-interventional approach (20,21). Conservative management includes maintaining hemodynamic status by fluid resuscitation or blood product replacement and careful observation. In appropriate cases, close follow-up as an outpatient can be attempted. Conversely, there is a higher failure rate of non-operative management with subsequent surgical repair in cases of a higher grade of injury. Splenic artery angiography with embolization is a viable alternative to surgical intervention in patients who are hemodynamically capable of tolerating the angiography (22). Although one previous publication found a 93% success rate in patients with traumatic spleen injury with angiography, results of angiography in colonoscopically induced injury has been mixed (9,23). Hemodynamically unstable patient should be taken for operative management. Ultimately, treatment option will likely be interdisciplinary, depending on the clinician’s preference, availability of treatment modality and operator technical proficiency.
Acknowledgement
We would like to thank Jennifer H. Lee, MFA, for her assistance.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- Seeff LC, Richards TB, Shapiro JA, et al. How many endoscopies are performed for colorectal cancer screening? results from CDC’s survey of endoscopic capacity. Gastroenterology 2004;127:1670-77. [Crossref] [PubMed]
- Centers for Disease Control and Prevention (CDC). Vital signs: Colorectal cancer screening test use--united states, 2012. MMWR Morb Mortal Wkly Rep 2013;62:881-8. [PubMed]
- Whitlock EP, Lin JS, Liles E, et al. Screening for colorectal cancer: A targeted, updated systematic review for the US preventive services task force. Ann Intern Med 2008;149:638-58. [Crossref] [PubMed]
- Fisher DA, Maple JT, Ben-Menachem T, et al. Complications of colonoscopy. Gastrointest Endosc 2011;74:745-52. [Crossref] [PubMed]
- Rabeneck L, Paszat LF, Hilsden RJ, et al. Bleeding and perforation after outpatient colonoscopy and their risk factors in usual clinical practice. Gastroenterology 2008;135:1899-906. [Crossref] [PubMed]
- Jehangir A, Poudel DR, Masand-Rai A, et al. A systematic review of splenic injuries during colonoscopies: Evolving trends in presentation and management. Int J Surg 2016;33:55-9. [Crossref] [PubMed]
- Kamath AS, Iqbal CW, Sarr MG, et al. Colonoscopic splenic injuries: Incidence and management. J Gastrointest Surg 2009;13:2136-40. [Crossref] [PubMed]
- Rosati C, Ata A, Siskin GP, et al. Management of splenic trauma: A single institution’s 8-year experience. Am J Surg 2015;209:308-14. [Crossref] [PubMed]
- Piccolo G, Di Vita M, Cavallaro A, et al. Presentation and management of splenic injury after colonoscopy: A systematic review. Surg Laparosc Endosc Percutan Tech 2014;24:95-102. [Crossref] [PubMed]
- Petersen CR, Adamsen S, Gocht-Jensen P, et al. Splenic injury after colonoscopy. Endoscopy 2008;40:76-9. [Crossref] [PubMed]
- Biecker E. A (not so) rare complication of colonoscopy. Gastroenterology 2016;151:e18-9. [Crossref] [PubMed]
- Skipworth JR, Raptis DA, Rawal JS, et al. Splenic injury following colonoscopy-an underdiagnosed, but soon to increase, phenomenon? Ann R Coll Surg Engl 2009;91:W6-11. [Crossref] [PubMed]
- Ha JF, Minchin D. Splenic injury in colonoscopy: A review. Int J Surg 2009;7:424-7. [Crossref] [PubMed]
- Shankar S, Rowe S. Splenic injury after colonoscopy: Case report and review of literature. Ochsner J 2011;11:276-81. [PubMed]
- Lauretta A, Busuito G, Bellomo RE. Splenic injury during colonoscopy: A complication hardly thought hence hardly sought. Am Surg 2014;80:E111. [PubMed]
- Federle MP, Goldberg HI, Kaiser JA, et al. Evaluation of abdominal trauma by computed tomography. Radiology 1981;138:637-44. [Crossref] [PubMed]
- Moore EE, Cogbill TH, Jurkovich GJ, et al. Organ injury scaling: Spleen and liver (1994 revision). J Trauma 1995;38:323-4. [Crossref] [PubMed]
- Schurr MJ, Fabian TC, Gavant M, et al. Management of blunt splenic trauma: Computed tomographic contrast blush predicts failure of nonoperative management. J Trauma 1995;39:507-12; discussion 512-3. [Crossref] [PubMed]
- Chiu WC, Cushing BM, Rodriguez A, et al. Abdominal injuries without hemoperitoneum: A potential limitation of focused abdominal sonography for trauma (FAST). J Trauma 1997;42:617-23; discussion 623-5. [Crossref] [PubMed]
- Peitzman AB, Heil B, Rivera L, et al. Blunt splenic injury in adults: Multi-institutional study of the eastern association for the surgery of trauma. J Trauma 2000;49:177-87; discussion 187-9. [Crossref] [PubMed]
- Prowda JC, Trevisan SG, Lev-Toaff AS. Splenic injury after colonoscopy: Conservative management using CT. AJR Am J Roentgenol 2005;185:708-10. [Crossref] [PubMed]
- Haan JM, Bochicchio GV, Kramer N, et al. Nonoperative management of blunt splenic injury: A 5-year experience. J Trauma 2005;58:492-8. [Crossref] [PubMed]
- Hagiwara A, Yukioka T, Ohta S, et al. Nonsurgical management of patients with blunt splenic injury: Efficacy of transcatheter arterial embolization. AJR Am J Roentgenol 1996;167:159-66. [Crossref] [PubMed]
Cite this article as: Li S, Gupta N, Kumar Y, Mele F. Splenic laceration after routine colonoscopy, a case report of a rare iatrogenic complication. Transl Gastroenterol Hepatol 2017;2:49.


