Left hepatectomy with simultaneous hepatic artery and portal vein reconstructions in the operation for cholangiocarcinoma: the surgical techniques comprised of step-by-step established procedures
Introduction
Hilar cholangiocarcinoma occasionally invades adjacent hepatic arteries, which necessitates hepatic artery reconstructions for a curative resection. Cancer involvement of the hepatic arteries often accompanies simultaneous involvement of the portal vein. Therefore, in cholangiocarcinoma operation with a hepatic artery reconstruction, a simultaneous portal vein reconstruction is often needed. Miyazaki et al. reported the high incidence of serious postoperative complications in cholangiocarcinoma operation with a hepatic artery reconstruction (1). Thus, they concluded that such operations could not be justified. On the other hand, Nagino et al. (2) reported the acceptable mortality of cholangiocarcinoma operation with simultaneous resections and reconstructions of the portal vein and the hepatic artery. Nevertheless, this operation is one of the most complicated and the most challenging ones in abdominal surgeries. Most of the hepatectomies with simultaneous hepatic artery and portal vein reconstructions are left-sided because of anatomical reasons. Although this type of operation consists of many steps, each step is merely one of well-established procedures. We present here our step-by-step procedures for left hepatectomy with simultaneous resections and reconstructions of the hepatic artery and the portal vein in cholangiocarcinoma operation.
Patients
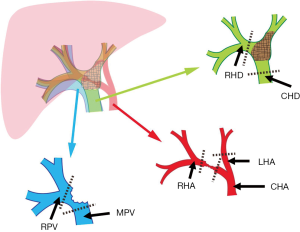
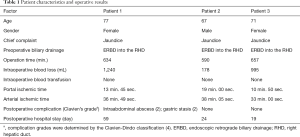
Two patients had Bismuth type III b hilar cholangiocarcinoma (3) and one patient had intrahepatic cholangiocarcinoma, all of which directly invaded not only the hepatic artery but also the portal vein (Figure 1). The mode of invasion necessitated simultaneous resection and reconstruction of the hepatic artery and the portal vein for curative resection. The characteristics and the preoperative information of these patients are summarized in Table 1.
Full table
Surgical techniques
There were 15 main steps in this operation:
- Tape-control of the right hepatic artery (RHA) at the porta hepatis (securing the peripheral anastomotic margin for hepatic artery anastomosis);
- Tape-control of the right portal vein (RPV) at the porta hepatis (securing the peripheral anastomotic margin for portal vein anastomosis);
- Tape-control of the proper hepatic artery proximal to the cancer involvement;
- Tape-control of the main portal vein (MPV) proximal to the cancer involvement;
- Dissection of the gallbladder from the liver bed;
- Transection of the common bile duct just above the pancreas;
- Counterclockwise rotation of the Spiegel lobe by dividing the left inferior vena cava ligament and the short hepatic veins;
- Parenchymal transection between the right and left hemilivers using a liver hanging maneuver;
- Division of the right hepatic duct (RHD) by subtracting the RHA and the RPV;
- Division of the RHA and the proper hepatic artery;
- Division of the RPV and the MPV;
- Division of the left hepatic vein using a stapler;
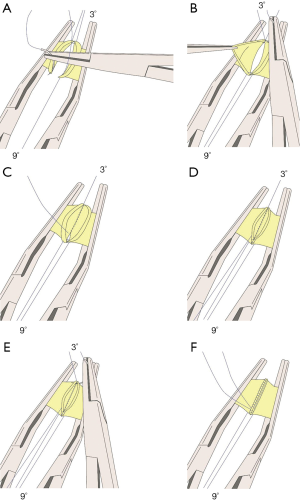
- Reconstruction of the portal vein by directly anastomosing the RPV and the MPV;
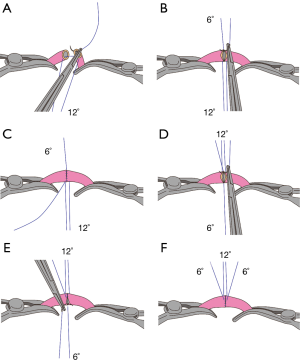
- Reconstruction of the hepatic artery by directly anastomosing the RHA and the proper hepatic artery;
- Biliary reconstruction by hepaticojejunostomy.
The detailed surgical procedures were as follows.
The abdomen was opened through bilateral subcostal incisions with a midline extension. The abdominal cavity was thoroughly inspected in order to confirm there was neither liver metastasis nor peritoneal dissemination. First, an attempt to encircle the RHA and the RPV by vascular tapes at the porta hepatis (peripheral to the cancer involvement) was made because the inability of this attempt meant that it was impossible to reconstruct the RHA and the RPV, which meant that the cancer could not be resected. After this attempt was successfully achieved, the proper hepatic artery and the MPV proximal to the cancer involvement were controlled with vascular tapes. After these first and the second attempts were successfully achieved, the extent of the cancer involvement to the vascular structure was confirmed by gross inspection. The gallbladder was freed from the gallbladder bed, dividing the cystic artery. The common bile duct was divided just above the pancreas. The distal stump of the common bile duct was brought up in order for the surgeons to further inspect the cancer involvement to the hepatic artery and the portal vein. The Spiegel lobe was rotated counterclockwise by dividing the inferior vena cava ligament and the short hepatic veins. Parenchymal transection between the right and left hemilivers was achieved using an ultrasonic aspiration dissector and soft coagulation. The RHD was divided at the point that seemed to be freed from cancer involvement. The RHA and the proper hepatic artery were meticulously trimmed at the dividing points for prompt reconstruction of the RHA after the specimen removal. The RHA and the proper hepatic artery, and then the RPV and the MPV were divided at the proximal and distal points that were freed from the cancer involvement (Figure 1). Finally, after the left hepatic vein (the confluence of the left and middle hepatic veins in patient 3 due to the cancer involvement to the middle hepatic vein) was divided using a stapler, the specimen was removed from the operative field. First, the portal vein reconstruction was achieved as shown in Figure 2. Then the RHA was reconstructed as shown in Figure 3 under loupe magnification. Biliary reconstruction was achieved by hepaticojejunostomy (Figure 4).
Operative results
The operative results are summarized in Table 1. No intraoperative blood transfusion was administered in all the patients. The mean portal and arterial ischemic time of the remnant liver was 14 min. 32 sec. and 35 min. 58 sec., respectively. The mean operative time and the intraoperative blood loss in the three patients were 627 min. and 804 mL, respectively. Only patient 1 experienced postoperative complications. She suffered intraabdominal abscess and gastric stasis both of which healed without any invasive intervention.
Discussion
Complications related to vascular anastomosis often lead to serious morbidity (1). Hepatic artery thrombosis or stenosis may lead to insufficient arterial blood circulation in the remnant liver. Because the biliary tract system in the liver is mainly nourished by arterial blood supply, insufficient arterial blood circulation in the remnant liver often leads to intrahepatic abscess formation caused by necrosis of the biliary tract, and occasionally leads to the disruption of the biliary anastomosis. On the other hand, an inappropriate reconstruction of the portal vein may occasionally lead to portal vein thrombosis, which results in various types of postoperative complications. The key point of this operation resides in how both the hepatic artery and the portal vein reconstructions are successfully accomplished. In order to avoid kinking at the anastomosis, vascular clamps are always applied in the same manner as shown in Figure 2 and Figure 3 (from the 9 o’clock direction for the portal vein and from the 12 o’clock direction for the hepatic artery). In order to avoid prolonged arterial ischemia of the remnant liver, we reconstructed hepatic arteries with 7-0 running sutures under loupe magnification. The mean arterial ischemic time was approximately 35 min. in this series. Some investigators advocated the use of microscope for hepatic artery reconstructions in this type of operation (1,2,6). However, the outer diameter of the proper hepatic artery is approximately 5 mm. which is too large to be anastomosed under microscope. For this size of hepatic arteries, the magnification by surgical loupes seems to be sufficient. Our procedure for hepatic artery reconstruction enables surgeons to more promptly reconstruct hepatic arteries without time consuming skills (the techniques of microvascular surgery need special training). We believe the shorter the total arterial ischemic time, the lesser the postoperative complications such as bile leakage and abscess formation would occur.
When a direct end-to-end anastomosis between the RHA and the proper hepatic artery cannot be achieved because of the gap between these two arteries, the gastroduodenal artery and the right gastroepiploic artery will become another candidate inflow artery (7). Surgeons have to check the usefulness of these arteries on imaging studies preoperatively. On the other hand, a gap between the RPV and the MPV for a direct anastomosis may hardly be problematic in this type of operation. Patients with far progressive cancer invasion to the portal vein in which a direct anastomosis between the RPV and the MPV cannot be performed may hardly become a candidate for cholangiocarcinoma operation.
Will hepatectomy with simultaneous hepatic artery and portal vein reconstructions for patients with Bismuth type III a or IV, namely right hepatectomy, left trisegmentectomy, or right trisegmentectomy with simultaneous hepatic artery and portal vein reconstruction, become a standard operation like the operation presented here? The answer is probably no. From purely oncological and anatomical perspectives, there exist very few cases of hilar cholangiocarcinoma for which right hepatectomy, or right trisegmentectomy with simultaneous hepatic artery and portal vein reconstruction would be performed with curative intent. On the other hand, there seem to exist more cases for left trisectionectomy with simultaneous hepatic artery and portal vein reconstruction considering the vascular anatomy in the hepatic hilum. However, the hepatic artery reconstruction in trisectionectomy needs an anastomosis between the posterior branch of the RHA and some inflow artery. The stump of the posterior branch of the RHA is not only short but also very thin. Therefore, it is much more difficult to reconstruct the posterior branch of the RHA than to reconstruct the main RHA. In addition, there are many anatomical variations at the level of this artery. Therefore, left trisectionectomy with hepatic artery and portal vein reconstructions is much more technically demanding than left hepatectomy with hepatic artery and portal vein reconstructions.
In conclusion, left hepatectomy with simultaneous hepatic artery and portal vein reconstructions is simply composed of step-by-step well-established procedures. Therefore, this type of operation could be standardized.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Miyazaki M, Kato A, Ito H, et al. Combined vascular resection in operative resection for hilar cholangiocarcinoma: does it work or not? Surgery 2007;141:581-8. [Crossref] [PubMed]
- Nagino M, Nimura Y, Nishio H, et al. Hepatectomy with simultaneous resection of the portal vein and hepatic artery for advanced perihilar cholangiocarcinoma: an audit of 50 consecutive cases. Ann Surg 2010;252:115-23. [Crossref] [PubMed]
- Bismuth H, Nakache R, Diamond T. Management strategies in resection for hilar cholangiocarcinoma. Ann Surg 1992;215:31-8. [Crossref] [PubMed]
- Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205-13. [Crossref] [PubMed]
- Uchiyama H, Shirabe K, Araki K, et al. The representative left hepatectomy with simultaneous hepatic artery and portal vein reconstructions in the operation for cholangiocarcinoma. Asvide 2017;4:183. Available online: http://www.asvide.com/articles/1491
- Shimada H, Endo I, Sugita M, et al. Hepatic resection combined with portal vein or hepatic artery reconstruction for advanced carcinoma of the hilar bile duct and gallbladder. World J Surg 2003;27:1137-42. [Crossref] [PubMed]
- Uchiyama H, Shirabe K, Morita M, et al. Expanding the applications of microvascular surgical techniques to digestive surgeries: a technical review. Surg Today 2012;42:111-20. [Crossref] [PubMed]
Cite this article as: Uchiyama H, Shirabe K, Araki K, Sugimachi K, Morita K, Takenaka K, Maehara Y. Left hepatectomy with simultaneous hepatic artery and portal vein reconstructions in the operation for cholangiocarcinoma: the surgical techniques comprised of step-by-step established procedures. Transl Gastroenterol Hepatol 2017;2:34.


