A rare case of retroperitoneal paraganglioma—case report and literature review
Disease history
A 19-year-old female patient was admitted due to “headache and elevated blood pressure for 2 months”. She had suffered from occasional headaches and dizziness 2 months before. The highest blood pressure during the onset of symptoms was 170/100 mmHg. However, there were no symptoms such as facial flushing, excessive sweating, nausea/vomiting, or blurred vision. Abdominal MRI in our hospital (Figures 1-6) suggested the possibilities of “retroperitoneal tumor” or “pheochromocytoma”. The 24-hour urine test performed in Peking Union Medical College (PUMC) Hospital showed that the secretion of norepinephrine significantly increased, and somatostatin receptor scintigraphy (SRS) (Figure 7) revealed retroperitoneal high contrast medium intake. The possibilities of “neuroendocrine tumor” or “paraganglioma” were considered. Phenoxybenzamine (10 mg bid po) was then administered to maintain the blood pressure at about 110/70 mmHg. She was hospitalized for surgery. She had no other history of disease. Physical examinations did not show any positive sign.
Auxiliary examination
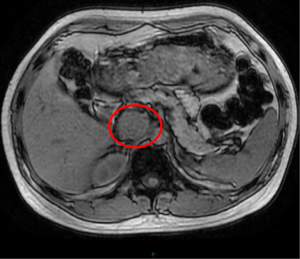
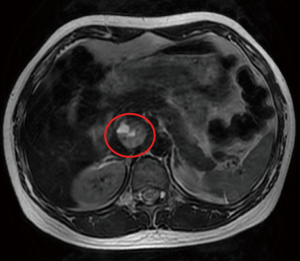
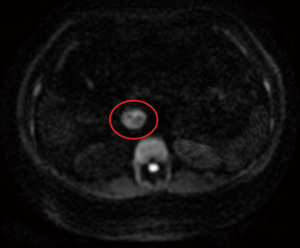
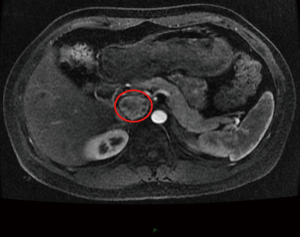
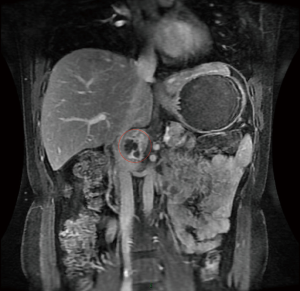
Abdominal MRI (June 2015, in our hospital): A spherical mass was found in the front of right kidney in the retroperitoneal region. The mass sized about 2.9 cm × 2.9 cm × 3.6 cm and had a clear margin. It showed slightly low signal (with spotty high signal) on dual-echo T1WI (Figure 1). The signal was not significantly lower in the out-of-phase than in the in-phase. Intermediate and high signals with internal regular patchy bright signal were shown on both T2WI/FS and T2WI (Figure 2). It showed high signal intensity on DWI (Figure 3). Contrast-enhanced scan showed marked enhancement of the solid portions, whereas there was no enhancement in the cystic areas (Figure 4). It was located among portal vein, inferior vena cava, and left renal vein, compressing the inferior vena cava to move rightwards (Figures 5,6). The possibility of “ectopic pheochromocytoma” was considered.
The 24-hour urine test in PUMC Hospital in August 2015 showed that the norepinephrine level was 597.92 µg/24 h (normal range, 16.69–40.65 µg/24 h).
ECG in our hospital in August 2015 prompted sinus arrhythmia/ST-T wave changes.
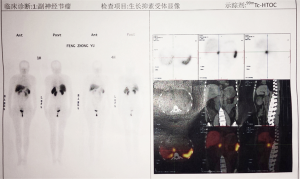
SRS in Peking Union Medical College Hospital in August 21, 2015: a relatively large soft tissue mass was seen at the T12–L1 levels, with remarkably increased radioactive iodine uptake (Figure 7). Thus, the retroperitoneal mass had high somatostatin receptor expression, and a neuroendocrine tumor (possibly paraganglioma) was considered. No other obvious abnormality was seen in SRS.
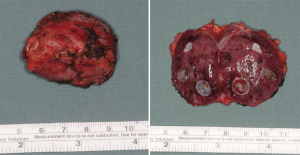
The retroperitoneal tumor was removed on September 8, 2015, and the postoperative samples were shown in the Figure 8.
Morphology: the tumor was sized 4 cm × 2.8 cm × 3 cm, with intact capsule. The cut surface was solid, tough, and gray-brown in color (Figure 8). Vesicle formation was seen in focal lesions, with suspicious bleeding. No gray-white and solid area was identified.
Post-operative pathology: based on the tumor site as well as morphological and immunohistochemical findings, a paraganglioma in extra-adrenal sympathetic nerve (located on the upper and lower sides near the aorta) was confirmed. The tumor tissue was actively growing, with abundant cells. In some areas the tumor tissues were diffusely growing, with remarkable cellular atypia, among which prominent nucleoli were observed, along with occasionally visible mitotic figures [0–1/50 high-power field (HPF)] and a pathological mitotic figure. The focal lesions involved the capsule, which should be closely followed up. The lymph nodes showed chronic inflammation but without metastatic tumor (0/4: hilar lymph node, 0/1; retroperitoneal tumor lymphs around the tumor: 0/3). Immunohistochemistry showed: AE1/AE3(−), CK18(−), S100(+++), ChrA(+++), Syno(+++), cd56(+++), and Ki-67<5%.
Discussion
Relationship between paraganglioma and pheochromocytoma/neuroendocrine tumors
Neuroendocrine tumors refer to all tumors arising from neuroendocrine cells. After amine precursor uptake and decarboxylation, these cells can produce peptides or active amines. Neuroendocrine tumors are highly heterogeneous due to their locations and secretion function. Among them, pheochromocytoma is a tumor with relevant clinical symptoms due to the excessive secretion of catecholamine. The vast majority of chromaffin cells are located in the adrenal gland. In fact, the adrenal medulla is a special type of paraganglia; thus, tumors arising from the adrenal medulla are also known as pheochromocytoma. Thus, the pheochromocytomas arising outside the adrenal gland is called paraganglioma, which is mostly seen in thoracic and abdominal sympathetic nerves. More specifically, the retroperitoneal paraganglioma accounts for over 50% of all paragangliomas and the functional paraganglioma 15–24%.
Clinical examinations required to confirm the diagnosis of paraganglioma
The common manifestations of paraganglioma include a series of sympathetic hyperactivity-related symptoms such as paroxysmal hypertension and metabolic disorders, which is mainly due to the increase of blood catecholamine level. Plasma and urine metanephrines (MNs) and 24-hour urine vanillylmandelic acid (VMA) levels may also rise. Determination of blood norepinephrine, epinephrine, and dopamine has been found to be the most sensitive method. The 24-hour urine norepinephrine level remarkably escalated in this patient, showing certain diagnostic significance. The 131I-Iobenguane has shown a high specificity in localizing paraganglioma and thus can be used for localization. After the tumor was localized, a second CT or MRI was performed to confirm the tumor size and its relationships with adjacent tissues. In addition, pheochromocytoma/paraganglioma was also one of type II multiple endocrine neoplasia (MEN II). Therefore, after a paraganglioma is confirmed, the presence of any neuroendocrine tumor should also be identified. Similar to other neuroendocrine tumors, paraganglioma also has highly expressed somatostatin receptors such as SSTR2 and SSTR3 (1,2). The presence of somatostatin receptors is helpful to identify systemic lesions. Janssen et al. (3).found that [68Ga]-DOTATATE PET/CT had a better localization value for SDHB-related metastatic paraganglioma. SRS in our current patient showed that somatostatin receptor were highly uptaken in the original primary lesion but not accumulated in other sites, suggesting that it was a single lesion.
Malignancy and distant metastasis of paraganglioma
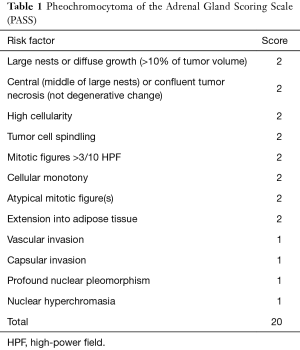
Pheochromocytoma/paraganglioma is a relatively rare disease, with a crude prevalence of 2 per 100,000 person/year (4) due to its low prevalence, no definite diagnostic criteria have been available to distinguish benign and malignant lesion. Cellular atypia may be not obvious in some malignant tumors, whereas remarkable atypia or multinucleated tumor giant cells may be seen in some benign tumors; even the capsular infiltration or vascular invasion can not confirm the presence of a malignant lesion. Thus, a malignancy can be confirmed only if there is a definite diffuse infiltration of surrounding organs/tissues or distant metastasis. Thompson et al. (5) retrospectively analyzed the data of 100 pheochromocytoma cases and proposed a Pheochromocytoma of the Adrenal Gland Scaled Score (Table 1). In this system the risk factors include tumor necrosis, capsular/vascular invasion, extension into to tissues adjacent to adrenal gland, large/dilated/fused nests, diffuse growth of tumor, increased cell components, tumor cell spindling, profound cellular and nuclear pleomorphism, cellular monotony, big nucleolus, increased mitotic figure >3/10 HPF, atypical mitotic figure, and lack of transparent balls. Pheochromocytoma with a total PASS score of <4 is regarded as benign and those with a PASS score of ≥4 are considered to be tumors with a potential for malignancy. The PASS score was >4 in our patient, which was highly suggestive of malignancy. Life-time follow-up was recommended. However, the precision of this scale still requires further verification. Wu et al. (6) invited pathologists with rich experiences to carry out risk assessment of tumors using this scale and found the results showed marked heterogeneity among different observers. Thus, this system is not recommended for assessing clinical prognosis. The incidence of malignant change among retroperitoneal paraganglioma reportedly ranges from 14% to 50% (7), with a 5-year overall survival rate of about 50%. In particular, patients with SDHB mutation can have even poorer prognosis, with a 5-year survival rate of about 36%; in contrast, the 5-year survival rate was about 67% in patients with negative SDHB mutation (8). A recent retrospective study (4) showed that the proportion of malignant change was higher in paraganglioma group than among pheochromocytoma group. After a median 80 months of follow-up, 3 and 5 death cases were noted in the pheochromocytoma group and paraganglioma group, respectively. Notably, the 5- and 10-year survival rates were 91% and 83% in the paraganglioma group.
Full table
Treatment
Similar to pheochromocytoma, surgery is the preferred treatment for paraganglioma. Phenoxybenzamine should be orally administered 6 weeks before surgery to relieve symptoms. The operation should be gentle to avoid wild fluctuations in blood pressure. Water-electrolyte balance should be maintained after the surgery, and any risk of adrenal crisis should be avoided. Radionuclide therapy and systemic chemotherapy has been reportedly used for malignant paraganglioma with distant metastasis. Ayala-Ramirez (9) retrospectively analyzed the clinical data of 52 patients with pheochromocytoma or paraganglioma with distant metastasis who had received systemic chemotherapy. Among them the most commonly used protocol was CVD (cyclophosphamide + vincristine + dacarbazine), with an objective response rate of 33%. Patients responsive to chemotherapy had a median survival time of 6.4 years, which was significantly superior to that (3.7 years) in non-responsive patients. In addition, compared with chemotherapy alone, resection of the primary tumor + systemic chemotherapy could significantly prolong the median survival (3.0 vs. 6.5 years). Ezzat Abdel-Aziz et al. (4) reported that, in patients with malignant paraganglioma, the median time to recurrence after the surgery was 38 months, with bone, liver, and lungs being the most commonly involved organs. In these patients, 90Y-DATA-labelled octreotide can achieve a response rate of 37–78% (4,8). There were several case reports on the application of molecularly targeted drugs (e.g., sunitinib and everolimus) in the treatment of this disease; however, the long-term efficacy remained unsatisfactory, and further clinical studies are warranted to clarify their roles.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Elston MS, Meyer-Rochow GY, Conaglen HM, et al. Increased SSTR2A and SSTR3 expression in succinate dehydrogenase-deficient pheochromocytomas and paragangliomas. Hum Pathol 2015;46:390-6. [Crossref] [PubMed]
- Reubi JC, Waser B, Schaer JC, et al. Somatostatin receptor sst1-sst5 expression in normal and neoplastic human tissues using receptor autoradiography with subtype-selective ligands. Eur J Nucl Med 2001;28:836-46. [Crossref] [PubMed]
- Janssen I, Blanchet EM, Adams K, et al. Superiority of [68Ga]-DOTATATE PET/CT to Other Functional Imaging Modalities in the Localization of SDHB-Associated Metastatic Pheochromocytoma and Paraganglioma. Clin Cancer Res 2015;21:3888-95. [Crossref] [PubMed]
- Ezzat Abdel-Aziz T, Prete F, Conway G, et al. Phaeochromocytomas and paragangliomas: A difference in disease behaviour and clinical outcomes. J Surg Oncol 2015;112:486-91. [Crossref] [PubMed]
- Thompson LD. Pheochromocytoma of the Adrenal gland Scaled Score (PASS) to separate benign from malignant neoplasms: a clinicopathologic and immunophenotypic study of 100 cases. Am J Surg Pathol 2002;26:551-66. [Crossref] [PubMed]
- Wu D, Tischler AS, Lloyd RV, et al. Observer variation in the application of the Pheochromocytoma of the Adrenal Gland Scaled Score. Am J Surg Pathol 2009;33:599-608. [Crossref] [PubMed]
- Cunningham SC, Suh HS, Winter JM, et al. Retroperitoneal paraganglioma: single-institution experience and review of the literature. J Gastrointest Surg 2006;10:1156-63. [Crossref] [PubMed]
- Andersen KF, Altaf R, Krarup-Hansen A, et al. Malignant pheochromocytomas and paragangliomas - the importance of a multidisciplinary approach. Cancer Treat Rev 2011;37:111-9. [Crossref] [PubMed]
- Ayala-Ramirez M, Feng L, Habra MA, et al. Clinical benefits of systemic chemotherapy for patients with metastatic pheochromocytomas or sympathetic extra-adrenal paragangliomas: insights from the largest single-institutional experience. Cancer 2012;118:2804-12. [Crossref] [PubMed]
Cite this article as: Li P, Zhao D. A rare case of retroperitoneal paraganglioma—case report and literature review. Transl Gastroenterol Hepatol 2016;1:58.