Chronic fibrous—degenerative pancreatitis with involvement of adjacent organs and their dysfunction: contemporary approaches to surgical treatment
Introduction
According to the classification by O. Shalimov, fibrous-degenerative pancreatitis with involvement of adjacent organs and their dysfunction is a separate form of chronic pancreatitis (CP) (1). Anatomic contact of the pancreas with adjacent organs in cases of progressing CP facilitates the development of extra pancreatic complications: duodenum evacuation disorder, biliary hypertension (BH), thrombosis or extravascular compression of splenoportomesenteric confluence veins (2). In cases of CP, bile duct stenosis and duodenal stenosis are caused by manifest pancreatic fibrosis and inflammation in the head of the pancreas (3). Some authors refer to the research by Beckerand Mischke, according to whom 19.5% out of 600 patients with CP understudy had a pathological state, which there searchers called groove pancreatitis. It is characterized by the appearance of adhesions between the pancreas and the duodenum, which leads to dysmotility, duodenal stenosis and tubular stenosis of bile ducts with the development of obstructive jaundice.
In cases of CP, obstruction of duodenum complicates the course of disease in 16.3–36.4% of patients; pre-papillary stenosis of the common bile duct (CBD) takes place in 30–59.6% of cases; and compression of the mesenteric-portal system with development of ascites occurs in 11.6–17.7% of patients (4,5).
Presently, there is no single opinion concerning the method preferable for surgical treatment of CP with dysfunction of adjacent organs. According to Begerand Büchler (5), the presence of stenosis of CBD and duodenum, and portal hypertension are the indications for isolated resection of the pancreas head (Beger’s procedure). According to the Resolution of the Plenary Session of the Board of the Hepato-Pancreato-Biliary Association of Russia and the CIS (Izhevsk 19–20 April 2012) (6), “…the scope of the initial operation of the pancreas in cases of complicated CP is determined by the nature and site of pathological changes, as well as the degree of functional impairment both on the part of the pancreas itself and on the part of adjacent organs and structures. The aims of surgery should be as follows: possibly complete elimination of their reversibly changed areas of the gland, ensuring out flow of pancreatic juice from the remaining part of the organ, restoration of bile passage and patency of the portal vein, and elimination of duodenal stenosis”.
A certain role in development of obstructive jaundice in cases of CP is played also by constriction of the distal part of the CBD by fibrously-changed lingula of the pancreas (7). In such cases, to eliminate BH during the CP surgery, it is necessary to cut the lingula.
The problem of tactics in case of BH not accompanied by obstructive jaundice (whether to do a draining surgery, to apply biliodigestive anastomosis or biliopancreatic anastomosis) needs further research with application of magnetic-resonance cholangiopancreatography (MRCP) or endoscopic retrograde cholangiopancreatography (ERCP) in the preoperative period (8).
Surgical tactics for the treatment of CP accompanied by portal hypertension has not been utterly determined yet. Light and medium portal hypertension is an indication to resection surgeries (Beger, Frey’s) (9-11). Resection of the pancreas is technically complicated in cases of a grave portal hypertension with thrombosis in the system of the portal vein, and there is a high risk of intra operative hemorrhage (11,12). Therefore, a number of surgeons believe that portal hypertension is a counter-indication to any interventions on the pancreas (13).
Basing on the analysis of our own results, we are going to determine optimum methods of surgical treatment of CP with the involvement of adjacent organs and their dysfunction.
Methods
Surgical treatment was applied to 144 patients with complicated forms of CP at the department of general surgery of the Ivano-Frankivsk Regional Clinical Hospital in 2009–2016. Dysfunction of adjacent organs occurred in 54 (37.5%) cases, in particular (Table 1).
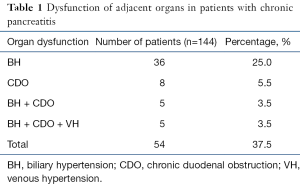
Full table
To diagnose the dysfunction of adjacent organs, we used laboratory tests (level of total and direct bilirubin, alkaline phosphatase), videoendoscopy of the stomach and duodenum, radioscopy of the stomach and the duodenum, ultrasonography (USG), ERCP, computed tomography (CT), MRCP, intraoperative measurement of bile passage diameter (IOMBPD), and intraoperative monitoring of biliary pressure (IOM BP) (use full model patent No. 101713, bul. No. 18 of 25.09.2015) (14). Assessment of remote results of surgical treatment was done by examining the patients, USG, laboratory tests, and filling out of the SF-36 questionnaire.
Results
Clinical manifestations of dysfunction of adjacent organs in patients with complicated forms of CP included both typical symptoms (pain syndrome, manifestations of endocrine and exocrine insufficiency), as well as symptoms of BH (jaundice, itching), and chronic duodenal obstruction (CDO) (heaviness in epigastrium, nausea, occasional vomiting). In particular, BH had clinical manifestations in 29 patients, and CDO—in 13 patients. Typical clinical symptoms of chronic portal-mesenteric obstruction were not registered.
Increased levels of total bilirubin (due to direct fraction) and alkaline phosphatase in blood serum were considered to be the markers of cholestatic conditions indicating to BH during laboratory examination. Particularly, hyperbilirubinemia connected with mechanical factor was found in 32 (69.6%) patients with BH, and hyperphosphatasemia—in 20 (43.5%) patients.
Enlarged and indurated head of the pancreas (from 3.5 to 5.3 cm) was found in all 54 patients during the ultrasonic diagnosis. Signs of BH (dilation of CBD from 0.8 to 1.7 cm) were diagnosed in 25 (46.3%) patients. In four (7.4%) patients, dilation of CBD was combined with intrapancreatic cysts of pancreas head; in another two (3.7%) patients—with parapancreatic cysts in the area of the head of the pancreas.
CT was applied in 35 (64.8%) cases. Enlarged and indurated head of pancreas was found in all patients. Cysts on the head of the pancreas were diagnosed by CT in three patients. Dilated suprapancreatic CBD occurred in 22 (62.85%) patients.
ERCP was applied to 11 (20.4%) patients, in whom CP was complicated by obstructive jaundice. Application of ERCP to another four patients was not possible due to manifest deformation of the duodenum, existence of a diverticulum or stenosis of the major duodenal papilla. Manifest tubular stenosis was found during ERCP in ten (90.9%) patients. In five patients, the examination ended by endobiliary stenting of the CBD. In addition, we found choledocholithiasis in one patient; he underwent papillosphincterotomy and concrement extraction.
To study the biliary tree and duct system of the pancreas, we applied MRCP to six patients with CP. Manifest tubular stenosis of intrapancreatic part of the CBD was found in all six patients. MRCP allowed determining precisely the length of strictures and their cause, which was of great practical value for the choice of surgical tactics (Figure 1).

According to the examination algorithm, all 54 patients of the study group underwent a videoendoscopic examination of the stomach and duodenum. In 13 patients who had clinical manifestations of CDO, it was confirmed endoscopically.
IOM BP during duodenum-preserving resections of the pancreas was applied to 24 patients. The tactics of surgical intervention depended on the results of BP monitoring. If BH remained after excision of fibrous tissues of the pancreas head and release of the intrapancreatic part of the CBD, the operation was supplemented by intervention on bile duct. If BH was eliminated by a surgery on the pancreas, intervention on bile passages was not applied.
All patients with CP received surgical treatment. The surgeries performed are characterized in Table 2.
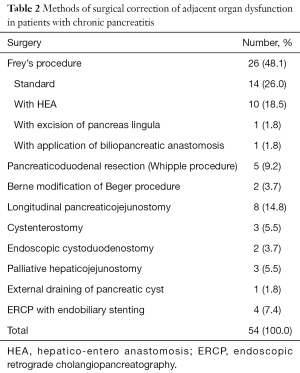
Full table
Frey’s procedure was used in 26 (48.1%) patients with CP complicated by the development of CDO, BH, or CDO + BH. Isolated damage of pancreas head by the fibrotic process and Wirsung’s duct ectasia without dysfunction of adjacent organs were considered the indications to the application of Frey’s procedure. In that case, it was necessary to remove a considerable part of the parenchymatous tissue of the pancreas head together with degeneratively changed nerve fibrils and intraparenchymal calcifications. Adequate excision of abnormal tissues was used to remove the inflamed tumor—a CP pacemaker; this allowed reaching decompression of small passages of the pancreas head and lesser pancreas. Counter—indications to Frey’s procedure included constriction of the upper mesenteric vein with the development of regional portal hypertension, duodenal dystrophy, and the impossibility to exclude malignant nature of the condition.
Frey’s procedure was performed in eight patients, in whom CP was complicated by CDO. Two patients underwent excision of fibrous tissues of the pancreas head together with cyst enucleation (in one patient—in the area of the lesser pancreas, in another patient—retroduodenal parapancreatic cyst). This intervention resulted in the elimination of CDO.
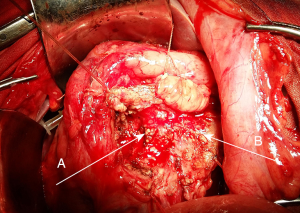
In six patients with CP accompanied by BH, removal of pathologically changed tissues of pancreas heads facilitated the elimination of BH; therefore, intervention on bile passages was not applied in these cases. In ten patients, Frey’s procedure was supplemented by application of hepatico-entero anastomosis (HEA) on a loop of the small bowel according to Roux; in two patients, pancreas lingual was excised; in one patient an internal biliopancreatic diversion was applied (Figure 2).
Beger procedure was applied in two (3.7%) patients with CP complicated by BH + CDO + venous hypertension (VH). It was performed in cases of CP with main damage of the head of the pancreas and little-changed passages of the body and tail of the pancreas. This intervention allowed eliminating all complications of CP.
In five (9.2%) patients, pancreaticoduodenal resection (PDR) according to Whipple was applied (Figure 3).
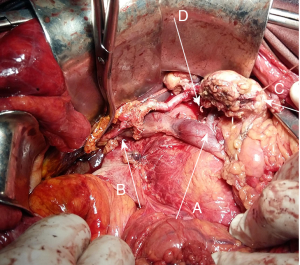
Indications to application of PDR in cases of chronic capitate pancreatitis included:
- Impossibility to exclude malignant process in pancreas head;
- Significantly enlarged head of pancreas, which caused CDO, BH, and VH simultaneously (three patients);
- Intrapancreatic cysts in the head of pancreas with a defect in the anterosuperior pancreaticoduodenal artery, which caused repeated hemorrhages into the lumen of a cyst and gastrointestinal tract (one patient). It was technically impossible to apply selective angiography and occlusion of the artery in that case.
Longitudinal pancreatic-enteric anastomosis (LPEA) was done in eight (14.8%) cases. Main indications for this surgery included the isolated Wirsung’s duct lithiasis, dilation of the main pancreatic duct without stenosis, occlusion of passages and significant fibrous degeneration of the pancreas head, and CP with atrophy of pancreas head and Wirsung’s duct ectasia. In all patients, the course of CP was complicated by BH; therefore, the operation was supplemented by application of HEA.
Due to the gravity of general condition or serious concomitant diseases, direct interventions on the pancreas were not applied in seven (12.9%) patients with CP accompanied by BH: HEA was applied in three (5.5%) cases; ERCP with endobiliary stenting was applied to four (7.4%) patients. Surgical treatment applied to them was not pathogenetic and did not eliminate the main substrate of the disease (fibrous-degenerative changes of pancreas head), as well as did not prevent the disease from progressing. However, they allowed eliminating BH.
The course of CP was complicated by BH caused by pseudocysts of the pancreas head and parapancreatic cysts in six (11.1%) patients. They underwent draining surgeries: open cystenterostomy on a loop according to Roux—in three (5.5%) patients, endoscopic cystoduodenostomy—in two (3.7%) patients, external draining of the pancreatic cyst—in one patient. These interventions sufficed to eliminate the BH.
The results of surgical treatment were traced in 23 (42.5%) patients with CP in the period from 6 to 36 months. According to the results of the questionnaire survey, all patients estimated their physical condition and psychoemotional state as good and satisfactory. The quality of life indicators in patients who underwent resection surgeries on the pancreas turned out to be the best while the quality of life indicators in patients after LPEA were much lower. As the vegetative syndrome and dyspeptic syndrome were more manifest in patients after PDR. However, objective research, laboratory and USG data show no signs of dysfunction of adjacent organs in these patients in the remote post-operative periods.
Conclusions
In the case of a complicated CP, the involvement of adjacent organs into the pathological process and their dysfunction is witnessed in 37.5% of cases.
The method of surgical intervention selected to treat patients with CP with involvement of adjacent organs and their dysfunction is duodenum-preserving resection surgery on the head of the pancreas, which in some cases needs to be supplemented by application of biliodigestive anastomoses or biliopancreatic diversions in the area of pancreas head resection in order to eliminate BH.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This paper has officially approved by ethical approval of Ethical Committee of Ivano-Frankivsk National Medical University (Ukraine).
References
- Shalimov AA, Shalimov SA, Nechitaylo ME, et al. Pancreatic surgery. Simferopol, 1997:506.
- Yareshko VG, Mikheyev YA. Selection of the method of surgical treatment of chronic pancreatitis and its complications. XXIII meeting of surgeons of Ukraine. Collection of scientific works, Kyiv 2015:219-20.
- Sebastiano PD, di Mola FF. Pathophysiology of Chronic Damage. In: Testoni PA, Mariani A, Arcidiacono PG, editors. Acute and Chronic Pancreatitis: New concepts and evidence-based approaches. Turin: Edizioni Minerva Medica, 2013:63-9.
- Dobrov SD, Polyakevich AS, Blagitko EM, et al. Biliary Hypertension in Chronic Pancreatitis Patients. Annaly khirurgicheskoy gepatologii 2012;17:35-40.
- Büchler MW, Baer HU, Seiler C, et al. Duodenum preserving resection of the head of the pancreas: a standard procedure in chronic pancreatitis. Chirurg 1997;68:364-8. [Crossref] [PubMed]
- Resolution of the Plenary Session of the Board of the Hepato-Pancreato-Biliary Association of Russia and the CIS (Izhevsk, 19-20 April 2012) “Chronic pancreatitis”. Annals of Surgical Hepatology 2012;17:118-9.
- Kopchak VM, Usenko AYU, Zelinskiy AI. Surgical anatomy of the pancreas. Kyiv 2011;141.
- Galperin EI, Diuzheva TG, Semenenko IA, et al. Remote results of isolated resection of the head of pancreas with decompression of pancreatic ducts in patients with chronic pancreatitic. Materials Plenum of the Association Surgeons-hepatologists of Russia and CIS countries; Izhevsk, 2002:13-5.
- Hirota M, Asakura T, Kanno A, et al. Long-period pancreatic stenting for painful chronic calcified pancreatitis required higher medical costs and frequent hospitalizations compared with surgery. Pancreas 2011;40:946-50. [Crossref] [PubMed]
- Agarwal AK, Raj Kumar K, Agarwal S, et al. Significance of splenic vein thrombosis in chronic pancreatitis. Am J Surg 2008;196:149-54. [Crossref] [PubMed]
- Ramesh H, Jacob G, Venugopal A, et al. Surgical management of chronic pancreatitis with portal hypertension--a 19-year experience. Surgery 2008;143:252-8. [Crossref] [PubMed]
- Bockhorn M, Gebauer F, Bogoevski D, et al. Chronic pancreatitis complicated by cavernous transformation of the portal vein: contraindication to surgery? Surgery 2011;149:321-8. [Crossref] [PubMed]
- Dominquez-Munoz E. Clinical pancreatology for practicing gastroenterologists and surgeons. Oxford: Blackwell publishing Ltd., 2007:535.
- Ivanovych PV, Mykhailovych KV, Mykhailovych IS, inventor; Ivano-Frankivsk National Medical University, State Higher Educational Institution. Method for surgical treatment of chronic pancreatitis complicated with cholelithiasis. Ukraine patent u201503315. 2015 Sep 4.
Cite this article as: Pylypchuk VI, Marino MV, Yavorskyy A. Chronic fibrous—degenerative pancreatitis with involvement of adjacent organs and their dysfunction: contemporary approaches to surgical treatment. Transl Gastroenterol Hepatol 2016;1:48.


