
Biliary hyperkinesia in adolescents—it isn’t all hype!
Introduction
The incidence of cholecystectomy in the pediatric population has increased considerably over the last several decades. This is likely due to a rise in childhood obesity, increased recognition of gallbladder pathology from widespread use of ultrasonography, and a change in physician perception of gallbladder disease (1-4). One of the most common indications for cholecystectomy in the pediatric population is biliary dyskinesia (5-7). Biliary dyskinesia is diagnosed in patients who have symptoms of biliary colic in the absence of stones with a depressed ejection fraction (EF) on a hepatobiliary iminodiacetic acid scan with cholecystokinin stimulation (CCK-HIDA testing). Performing cholecystectomies for biliary dyskinesia is helpful for symptom relief in pediatric patients (8-20). In addition, there is some literature to suggest that hyperkinetic gallbladders with elevated EFs greater than 65–80% can cause symptoms similar to classic biliary colic but this phenomenon is poorly understood. In total, there are only a few descriptions in both the adult and pediatric literature of this biliary hyperkinesia as a potentially surgically correctable disease (21-26). With improved descriptions of characteristics and outcomes for patients with hyperkinetic gallbladders, an understanding of optimal management will emerge. The aim of this present series is to describe the workup for this disease process and the outcomes associated with laparoscopic cholecystectomy for biliary hyperkinesia. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/tgh-20-258).
Methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by both Institutional Review Boards of Wake Forest School of Medicine (#IRB00000212) and UT Southwestern School of Medicine (#IRB00000974) and informed consent was taken from all the patients. We collected an observational database of children and adolescents (age ≤18), who underwent laparoscopic cholecystectomy for biliary hyperkinesia spanning over a 3-year period at two children’s hospitals. Age, sex, BMI, CCK-HIDA results, pre-operative esophagoduodenoscopy (EGD) findings (when present), post-operative pathology results and patient self-reported outcomes were obtained.
Inclusion criteria included patients ages ≤18 years old with a documented gallbladder EF of >80% on HIDA scan who underwent cholecystectomy for biliary hyperkinesia. Preoperative characteristics and work up were evaluated by chart review. Resolution of biliary colic symptoms was determined by documentation of subjective resolution of symptoms at the patients’ first postoperative follow up appointment. One patient was lost to follow up and was not included in the analysis of symptom resolution.
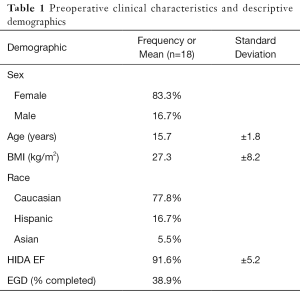
Descriptive statistics were utilized with the qualitative data reported in percentages and quantitative data reported in averages with standard deviations.
Results
During the study period, there were 187 pediatric patients (≤18 years old) who underwent workup and laparoscopic cholecystectomy by pediatric surgeons at the two tertiary care centers. Eighteen of these 187 patients had a documented gallbladder EF of >80% on HIDA scan. This group was predominantly (83.3%) female, Caucasian, and had a mean age of 15.7 years. The mean BMI was 27.3 (±8.2) kg/m2 (Table 1).
Full table
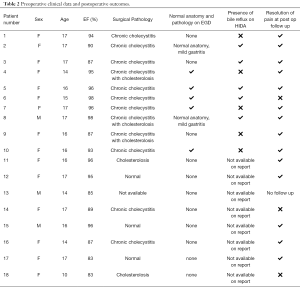
Preoperative clinical data and postoperative outcomes for our 18 patients can be seen in Table 2. Many of the patients had extensive medical work ups to determine the etiology of their abdominal pain prior to being referred for a surgical evaluation. Approximately one third (38.9%) of patients had an EGD prior to referral. All patients with preoperative EGD had this study performed prior to CCK-HIDA scan for workup of epigastric pain in the setting of normal right upper quadrant ultrasounds. All EGDs revealed normal gastric anatomy and the majority had normal biopsy pathology. Two EGD biopsies revealed mild gastritis. On CCK-HIDA scan, the average gallbladder EF was 91.6% (±5.2%). The HIDA scans were interpreted by several different nuclear medicine radiologists at each hospital and were not all interpreted by a single provider. Only ten of the imaging reports commented on the presence or absence of biliary reflux during the HIDA testing. Of those, 50% were noted to have biliary reflux into the stomach after sincalide was injected.
Full table
The large majority of patients (82.4%) had some degree of chronic cholecystitis or evidence of cholesterolosis on their gallbladder pathology results. Following cholecystectomy, the average time to follow up was 23.5 days. At follow up, 82.4% of the patients endorsed complete or near complete resolution of preoperative symptoms. One patient was lost to follow up and was not included in the analysis of symptom resolution.
Discussion
Chronic abdominal pain in children and adolescents is very common and often poses diagnostic and management challenges (27). Elucidating the cause of epigastric or right upper quadrant pain may prove to be difficult given the large differential. Gallbladder dysfunction is a common culprit as it is a highly complex system with both hormonal and autonomic input regulating gallbladder contraction and emptying (28). Any imbalance of these inputs can lead to the classic symptoms of biliary colic such as postprandial RUQ pain, nausea or vomiting. Biliary dyskinesia is commonly defined as symptoms of biliary colic in the absence of stones with a low HIDA scan EF (less than 35%). As previously described, these patients have been shown to respond well to surgical management (8-20). Conversely, biliary hyperkinesia is a less well understood and likely underreported diagnosis in adolescents that manifests with many of the same symptoms. As such, the clinical characteristics and response to surgical intervention with cholecystectomy remain largely undefined. A high percentage of patients (82.4%) in the present series experienced complete or near resolution of symptoms with cholecystectomy. Fourteen of 17 patients had postoperative pathology consistent with chronic cholecystitis and/or evidence of cholesterolosis. In addition, several of our patients had bile reflux noted on their HIDA scans, which may be an unrecognized source of pain in biliary hyperkinesia.
Previous literature has described biliary hyperkinesia as a gallbladder EF >65–80%. In the present series the majority of patients had EFs >90% (23-26).
Biliary hyperkinesia is likely an under diagnosed etiology of gallbladder pathology. Evidence of chronic inflammation was found on surgical pathology in almost all of our patients and 82.4% of the patients surveyed (n=17) experienced postoperative symptom relief. These findings are consistent with a study by Lindholm et al. of 12 pediatric patients with gallbladder EFs ≥ 80%. Similar to this present experience, all patients had evidence of cholecystitis on pathology and all patients endorsed symptomatic relief postoperatively (23). Conversely, a study by Dekonenko found that only 50% of pediatric patients (n=8) surveyed with an EF >65% had resolution of symptoms with the majority (63%) demonstrating evidence of chronic cholecystitis on pathology (24). While inflammation and mucosal irritation seem to be hallmarks of this process, the cause and effect is unclear. One current hypothesis is that intramural inflammation is due to the forceful contraction of gallbladder (25). This forceful contraction may be due to increased CCK receptor upregulation or signaling leading to increased sensitivity of the gallbladder to CCK. Hyper-responsiveness of gallbladder contraction and pressure generation may be exacerbated by failure of the Sphincter of Oddi to fully relax. The pressure increase of the biliary tree brought on by these two mechanisms may contribute to the pain experienced in patients with acalculous biliary colic. The gallbladder is effectively contracting against a closed system, thus pressurizing the ducts and eliciting pain (28) with an abrupt release in the pressurized gallbladder contents and forceful ejection of bile. Further evidence to support the theory of CCK signaling dysfunction contributing to this pathology comes from reports of those suffering from biliary colic who experience significant pain relief with use of a CCK receptor antagonist (29). Once the gallbladder is no longer contracting in response to CCK signaling, the symptoms abate. Karplus et al. attempted to determine the etiology of acalculous gallbladder dyskinesia in children by examining the histopathology of gallbladder tissue in patients with chronic acalculous gallbladder dysfunction (CAGD) as compared to controls. The CAGD group abnormally expressed the CCK receptor in the gallbladder mucosal epithelium, whereas normal receptor expression was seen only in the vascular epithelium and smooth muscle in the controls (30). Abnormal CCK receptor expression may play a role in both hypokinetic and hyperkinetic gallbladder dysfunction. Additional, pediatric patients with symptomatic cholelithiasis and traditional biliary dyskinesia have an increase in gallbladder mucosal mast cell density and activation (31,32) and a similar inflammatory process is likely occurring in the hyperkinetic gallbladder. However, Jones et al. evaluated the relationship between gallbladder pathology and gallbladder EF in children and adolescents and reported that gallbladder EF value did not correlate with any specific pathology (cholecystitis, cholelithiasis, cholesterolosis). Fifty-six of the 363 patients in that series had an EF >80% (33). Despite these robust numbers, the outcomes correlating symptom relief following cholecystectomy with surgical pathology in biliary hyperkinesia were limited and conflicting. Our series adds to the growing reports and suggests operative intervention is reasonable and often beneficial. Moreover, an underlying inflammatory process is likely the explanation for pain.
A number of studies evaluating the use of HIDA testing for traditional biliary dyskinesia propose that symptom onset during the CCK analog infusion is more predictive of postoperative symptom resolution than the EF value (34-37). Due to the inconsistent documentation of symptom re-creation on HIDA scan reports, we were unable to determine a correlation. However, it is unclear whether this data may have been instructive. A study by Dave et al. evaluating 100 patients with hypofunctioning gallbladders (EFs <35%) reported that neither reproduction of symptoms with CCK injection nor pathologic findings of cholecystitis were predictive of postoperative symptom relief (38). Yet, this lack of a CCK injection/pain correlation should be interpreted with caution as the context was patients with hypokinetic gallbladders and the findings may be different in those with EFs >80%. The majority of our patients experienced symptomatic relief and had EFs >90%. Further studies comparing EF value and postoperative symptomatic relief may help elucidate a clinically relevant relationship in patients with hyperkinetic gallbladders.
Even in the context of biliary colic symptoms and a high EF, it is important to rule out other forms of gastrointestinal pathology. Karnsakul et al. evaluated 16 children with acalculous biliary type abdominal pain with EFs <35% (39). All of the patients underwent upper endoscopy and the majority of patients (88%) had findings reflective of peptic acid disease. Over two-thirds of the patients underwent a two-week trial of proton pump inhibitor therapy with just less than half of the patients having complete resolution of symptoms without cholecystectomy. Seven of our 18 patients had pre-operative esophagogastroduodenoscopy. All revealed both normal anatomy and normal pathology, except for mild gastritis in 2 of the patients. Although the clinical entity of biliary hyperkinesia may be different from traditional biliary dyskinesia, it is important to highlight the importance of ruling out non-surgical causes of abdominal pain prior to operative intervention in both settings. Another potential source of abdominal pain is bile reflux. Duodenogastroesophageal reflux has been implicated in the development of GERD. Animal studies have demonstrated bile acids make mucosal cells increasingly susceptible to damage by gastric acid and pepsin (40,41). Bile reflux, which may be worsened after cholecystectomy, seems to augment H. pylori infections in harming gastric mucosa (42-44). If symptoms of GERD persist after acid suppression therapy, it is often due to bile reflux (41,45). Pre-operatively, ten patients had imaging reports which specifically commented on the presence or absence of bile reflux. Five of these 10 patients had duodenogastric reflux and this may be an unrecognized cause of pain. In these patients, it was not possible to discern if symptoms arose from biliary colic or duodenogastric reflux, as both would be exacerbated by postprandial gallbladder contraction. Further, vigorous contraction of a hyperkinetic gallbladder may worsen the concomitant bile reflux, but it might not be the sole cause of the retrograde flow in all cases. Further examination of the association between gallbladder dysfunction and duodenogastric reflux may help explain the pathophysiology of patients’ pain and why it is not always eliminated with surgical intervention.
The limitations of this study include the retrospective nature of the review which resulted in a small amount of data to collect due to differences in provider documentation. The median time to follow up was 24 days and long-term symptom resolution could not be assessed. Although our sample is the largest described cohort evaluating pediatric hyperkinesia, it is limited. To further advance the knowledge on this subject, multi-institutional prospective studies need to be performed in order to obtain satisfactory numbers. This would likely also require the creation of a standardized definition of biliary hyperkinesia and a universal preoperative workup to ensure other causes of abdominal pain were not present. This study highlights the multifactorial nature of pain in biliary hyperkinesia including CCK regulation, inflammatory processes, and coexistent duodenogastric reflux which should all be taken into consideration in future studies. The body of literature to inform continued research regarding biliary hyperkinesia remains limited.
Biliary hyperkinesia is an emerging clinical entity in children and adolescents and presents with many of the same symptoms of biliary colic noted in traditional biliary dyskinesia with hypokinetic gallbladders. While the pathophysiologic mechanism of pain is not fully elucidated, it does appear that laparoscopic cholecystectomy is beneficial for symptom resolution and should be considered for the difficult to treat abdominal pain with otherwise normal workup and history suggestive of biliary colic.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Translational Gastroenterology and Hepatology for the series “Current Topics in Pediatric General Surgery”. The article has undergone external peer review.
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/tgh-20-258
Data Sharing Statement: Available at http://dx.doi.org/10.21037/tgh-20-258
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tgh-20-258). The series “Current Topics in Pediatric General Surgery” was commissioned by the editorial office without any funding or sponsorship. SRP served as the unpaid Guest Editor of the series. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by both Institutional Review Boards of Wake Forest School of Medicine (#IRB00000212) and UT Southwestern School of Medicine (#IRB00000974) and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Waldhausen JH, Benjamin DR. Cholecystectomy is becoming an increasingly common operation in children. Am J Surg 1999;177:364-7. [Crossref] [PubMed]
- Kaechele V, Wabitsch M, Thiere D, et al. Prevalence of gallbladder stone disease in obese children and adolescents: influence of the degree of obesity, sex, and pubertal development. J Pediatr Gastroenterol Nutr 2006;42:66-70. [Crossref] [PubMed]
- Poffenberger CM, Gausche-Hill M, Ngai S, et al. Cholelithiasis and its complications in children and adolescents: update and case discussion. Pediatr Emerg Care 2012;28:68-76; quiz 77-78. [Crossref] [PubMed]
- Fradin K, Racine AD, Belamarich PF. Obesity and Symptomatic Cholelithiasis in Childhood: Epidemiologic and Case-Control Evidence for a Strong Relation. J Pediatr Gastroenterol Nutr 2014;58:102-6. [Crossref] [PubMed]
- Rothstein DH, Harmon CM. Gallbladder disease in children. Semin Pediatr Surg 2016;25:225-31. [Crossref] [PubMed]
- Mehta S, Lopez ME, Chumpitazi BP, et al. Clinical characteristics and risk factors for symptomatic pediatric gallbladder disease. Pediatrics 2012;129:e82-8. [Crossref] [PubMed]
- Bielefeldt K, Saligram S, Zickmund SL, et al. Cholecystectomy for Biliary Dyskinesia: How Did We Get There? Dig Dis Sci 2014;59:2850-63. [Crossref] [PubMed]
- Carney DE, Kokoska ER, Grosfeld JL, et al. Predictors of successful outcome after cholecystectomy for biliary dyskinesia. J Pediatr Surg 2004;39:813-6. [Crossref] [PubMed]
- Krishna YT, Griffin KL, Gates RL. Pediatric Biliary Dyskinesia: Evaluating Predictive Factors for Successful Treatment of Biliary Dyskinesia with Laparoscopic Cholecystectomy. Am Surg 2018;84:1401. [Crossref] [PubMed]
- Hofeldt M, Richmond B, Huffman K, et al. Laparoscopic cholecystectomy for treatment of biliary dyskinesia is safe and effective in the pediatric population. Am Surg 2008;74:1069. [Crossref] [PubMed]
- Constantinou C, Sucandy I, Ramenofsky M. Laparoscopic cholecystectomy for biliary dyskinesia in children: report of 100 cases from a single institution. Am Surg 2008;74:587. [Crossref] [PubMed]
- Michail S, Preud’Homme D, Christian J, et al. Laparoscopic cholecystectomy: Effective treatment for chronic abdominal pain in children with acalculous biliary pain. J Pediatr Surg 2001;36:1394-6. [Crossref] [PubMed]
- Dumont RC, Caniano DA. Hypokinetic gallbladder disease: A cause of chronic abdominal pain in children and adolescents. J Pediatr Surg 1999;34:858-61. [Crossref] [PubMed]
- Campbell BT, Narasimhan NP, Golladay ES, et al. Biliary dyskinesia: a potentially unrecognized cause of abdominal pain in children. Pediatr Surg Int 2004;20:579-81. [Crossref] [PubMed]
- Haricharan RN, Proklova LV, Aprahamian CJ, et al. Laparoscopic cholecystectomy for biliary dyskinesia in children provides durable symptom relief. J Pediatr Surg 2008;43:1060-4. [Crossref] [PubMed]
- Vegunta RK, Raso M, Pollock J, et al. Biliary dyskinesia: The most common indication for cholecystectomy in children. Surgery 2005;138:726-31. [Crossref] [PubMed]
- Gollin G, Raschbaum GR, Moorthy C, et al. Cholecystectomy for suspected biliary dyskinesia in children with chronic abdominal pain. J Pediatr Surg 1999;34:854-7. [Crossref] [PubMed]
- Kaye AJ, Jatla M, Mattei P, et al. Use of laparoscopic cholecystectomy for biliary dyskinesia in the child. J Pediatr Surg 2008;43:1057-9. [Crossref] [PubMed]
- Mahida JB, Sulkowski JP, Cooper JN, et al. Prediction of symptom improvement in children with biliary dyskinesia. J Surg Res 2015;198:393-9. [Crossref] [PubMed]
- Knott EM, Fike FB, Gasior AC, et al. Multi-institutional analysis of long-term symptom resolution after cholecystectomy for biliary dyskinesia in children. Pediatr Surg Int 2013;29:1243-7. [Crossref] [PubMed]
- Bates JA, Dinnan K, Sharp V. Biliary hyperkinesia, a new diagnosis or misunderstood pathophysiology of dyskinesia: A case report. Int J Surg Case Rep 2019;55:80-3. [Crossref] [PubMed]
- Huckaby L, Timmapuri S, Prasad R. Biliary hyperkinesia: A potentially surgically correctable disorder in adolescents. J Pediatr Surg Case Rep 2013;1:314-6. [Crossref]
- Lindholm EB, Alberty JB, Hansbourgh F, et al. Hyperkinetic gallbladder: an indication for cholecystectomy?. Am Surg 2013;79:882-4. [Crossref] [PubMed]
- Dekonenko C, Sujka JA, Dorman RM, et al. Self-reported Outcomes After Cholecystectomy for Pediatric Hyperkinetic Biliary Dyskinesia. J Surg Res 2020;246:73-7. [Crossref] [PubMed]
- Gazzetta J, Fan B, Bonner P, et al. Cholecystectomy for Biliary Hyperkinesia. Am Surg 2019;85:219-22. [Crossref] [PubMed]
- Saurabh S, Green B. Is hyperkinetic gallbladder an indication for cholecystectomy? Surg Endosc 2019;33:1613-7. [Crossref] [PubMed]
- Di Lorenzo C, Colletti RB, Lehmann HP, et al. Chronic Abdominal Pain In Children: A Technical Report of the American Academy of Pediatrics and the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition: AAP Subcommittee and NASPGHAN Committee on Chronic Abdominal Pain. J Pediatr Gastroenterol Nutr 2005;40:249-61. [Crossref] [PubMed]
- Grace PA, Poston GJ, Williamson RC. Biliary motility. Gut 1990;31:571-82. [Crossref] [PubMed]
- Malesci A, Pezzilli R, D’Amato M, et al. CCK-1 receptor blockade for treatment of biliary colic: a pilot study. Aliment Pharmacol Ther 2003;18:333-7. [Crossref] [PubMed]
- Karplus G, Ruiz R, Thomas DG, et al. Cholecystokinin receptor positivity in children with chronic acalculous gallbladder dysfunction: a pilot study to investigate the etiology of chronic acalculous gallbladder dysfunction. J Pediatr Surg 2008;43:850-3. [Crossref] [PubMed]
- Friesen CA, Neilan N, Daniel JF, et al. Mast cell activation and clinical outcome in pediatric cholelithiasis and biliary dyskinesia. BMC Res Notes 2011;4:322. [Crossref] [PubMed]
- Rau B, Friesen CA, Daniel JF, et al. Gallbladder wall inflammatory cells in pediatric patients with biliary dyskinesia and cholelithiasis: a pilot study. J Pediatr Surg 2006;41:1545-8. [Crossref] [PubMed]
- Jones PM, Rosenman MB, Pfefferkorn MD, et al. Gallbladder Ejection Fraction Is Unrelated to Gallbladder Pathology in Children and Adolescents. J Pediatr Gastroenterol Nutr 2016;63:71. [Crossref] [PubMed]
- Morris-Stiff G, Falk G, Kraynak L, et al. The Cholecystokin Provocation HIDA Test: Recreation of Symptoms is Superior to Ejection Fraction in Predicting Medium-Term Outcomes. J Gastrointest Surg 2011;15:345-9. [Crossref] [PubMed]
- Cofer JB, Dart BW 4th. Reproduction of postprandial symptoms with cholecystokinin injection: an indication for cholecystectomy without the presence of gallstones or an abnormal ejection fraction on quantitative cholescintigraphy? Am Surg 2007;73:689-92. [Crossref] [PubMed]
- DuCoin C, Faber R, Ilagan M, et al. Normokinetic biliary dyskinesia: a novel diagnosis. Surg Endosc 2012;26:3088-93. [Crossref] [PubMed]
- Carr JA, Walls J, Bryan LJ, et al. The Treatment of Gallbladder Dyskinesia Based Upon Symptoms. Surg Laparosc Endosc Percutan Tech 2009;19:222-6. [Crossref] [PubMed]
- Dave RV, Pathak S, Cockbain AJ, et al. Management of gallbladder dyskinesia: patient outcomes following positive 99mtechnetium (Tc)-labelled hepatic iminodiacetic acid (HIDA) scintigraphy with cholecystokinin (CCK) provocation and laparoscopic cholecystectomy. Clin Radiol 2015;70:400-7. [Crossref] [PubMed]
- Karnsakul W, Vaughan R, Kumar T, et al. Evaluation of gastrointestinal pathology and treatment in children with suspected biliary dyskinesia. Pediatr Surg Int 2011;27:1307-12. [Crossref] [PubMed]
- Katz PO. Review article: the role of non-acid reflux in gastro-oesophageal reflux disease. Aliment Pharmacol Ther 2000;14:1539-51. [Crossref] [PubMed]
- Tack J. Review article: the role of bile and pepsin in the pathophysiology and treatment of gastro-oesophageal reflux disease. Aliment Pharmacol Ther 2006;24:10-6. [Crossref] [PubMed]
- Zullo A, Rinaldi V, Hassan C, et al. Gastric Pathology in Cholecystectomy Patients: Role of Helicobacter pylori and Bile Reflux. J Clin Gastroenterol 1998;27:335-8. [Crossref] [PubMed]
- Mercan E, Duman U, Tihan D, et al. Cholecystectomy and duodenogastric reflux: interacting effects over the gastric mucosa. SpringerPlus 2016;5:1970. [Crossref] [PubMed]
- Chen SL, Mo JZ, Cao ZJ, et al. Effects of bile reflux on gastric mucosal lesions in patients with dyspepsia or chronic gastritis. World J Gastroenterol 2005;11:2834-7. [Crossref] [PubMed]
- Tack J, Koek G, Demedts I, et al. Gastroesophageal Reflux Disease Poorly Responsive to Single-Dose Proton Pump Inhibitors in Patients without Barrett’s Esophagus: Acid Reflux, Bile Reflux, or Both? Am J Gastroenterol 2004;99:981-8. [Crossref] [PubMed]
Cite this article as: Bosley ME, Jacobson J, Gaffley MWG, Beckwith MA, Pandya SR, Davis JS, Neff LP. Biliary hyperkinesia in adolescents—it isn’t all hype! Transl Gastroenterol Hepatol 2021;6:36.


