
Minimally invasive surgery of the pancreas: a narrative review of current practice
Background
Minimally invasive surgery for children with pancreatic pathology is a topic that is covered sporadically in the literature, with most information limited to case reports or case series. Newer trials evaluating strategies for management aim to capture the relatively small volume of patients with these issues by capitalizing on multi-institutional data sets. The information may be organized by specific pathology or by the type of operation used to ameliorate the problem. Herein we limit the discussion to the pathology most amenable to laparoscopy: distal pancreatectomy, subtotal pancreatectomy, enucleation and lateral pancreatojejunostomy. The intent of this manuscript is to give the reader an overview of the newest information available for a minimally invasive approach to the pancreas. We present the following article in accordance with the Narrative Review reporting checklist (available at http://dx.doi.org/10.21037/tgh-20-220).
Methods
We conducted a literature search on PubMed using the terms “minimally invasive surgery pancreas,” “pancreaticojejunostomy,” “Puestow,” “solid pseudopapillary tumor,” “pancreatic trauma,” and “hyperinsulinism” We included all manuscripts written in English spanning the time period between 1995 and 2020. Papers specific to children were selected for review.
Distal pancreatectomy
The minimally invasive distal pancreatectomy may be utilized in a number of clinical scenarios in the pediatric population including trauma, neoplasms and focal hyperinsulinism limited to the distal gland.
Traumatic pancreatic injury
In cases of traumatic transection of the main pancreatic duct following blunt injury, laparoscopic intervention may be utilized in the stable patient. Diagnosis of pancreatic injuries is typically a combination of cross-sectional imaging (MRI or CT) and endoscopic retrograde cholangiopancreatography (ERCP) or magnetic resonance cholangiopancreatography (MRCP). Pancreatic stents may be possible in transection of the mid-body of the pancreas, but more distal injuries are not well-suited to this intervention. These patients may recover faster following a definitive resection than with multiple failed interventions and pseudocyst formation. ERCP with stent placement that fails to traverse the point of ductal injury can lead to a functional island of pancreatic tissue distal to the transection. Further intervention such as distal pancreatectomy or cyst-gastrostomy may be indicated if the patient is symptomatic. Cyst-gastrostomy can be performed using endoscopic or laparoscopic techniques depending on the anatomic location of the cyst (1). Though non-operative management of solid organ injury is standard of care; the challenge is determining characteristics that predict failure of non-operative management. Major ductal disruption is particularly controversial. In their retrospective analysis of blunt pancreatic injuries treated at seven designated level 1 pediatric trauma centers in the US, Mattix et al. found that failure of non-operative management was significantly higher among patients with an injury grade III to V (2). Additionally, among patients with ductal injuries, those who failed non-operative management had significantly higher injury severity scores (2). The study was not sufficiently powered to detect a difference in recovery time between the two groups (2).
Non-operative management of pancreatic injuries in children is not without risk. In a series of 100 pediatric patients with pancreatic injury, 42% developed organized fluid collections, over half of which ultimately required intervention (3). Another review of operative versus non-operative management of pancreatic injury in children demonstrated a significantly higher proportion of patients with pseudocyst formation in those with the non-operative approach (4). Eleven percent of patients who had a distal pancreatectomy developed a leak, however all were controlled with the surgical drain placed at the initial operation (4). The laparoscopic approach to pediatric pancreatic injury appears to be safe. When comparing minimally invasive intervention to the open approach among 21 patients treated at six level 1 pediatric trauma centers, Iqbal et al. concluded that there was no difference in operative time, duration of hospital stay, or post-operative morbidity (4).
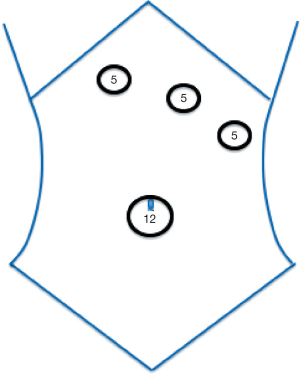
In contrast to adults, pediatric patients may be less likely to have associated intra-abdominal injuries (5). The increased frequency of isolated pancreatic injury in pediatric patients may relate to the difference in etiology. Children more frequently present after bicycle crashes whereas injuries in adults are more often a result of motor vehicle crashes (5). These isolated injuries lend themselves to minimally invasive surgical interventions. In a review of 200 pediatric patients with pancreatic injuries, the minimally invasive approach was shown to be a good diagnostic tool for patients with equivocal exam or imaging findings (6). Access to the abdomen is via the umbilicus and additional ports are oriented as for a splenectomy, since access to the splenic hilum is paramount to splenic preservation (Figure 1). Once the lesser sac is opened and the stomach retracted, key decision points include the method of taking the feeding venules between the posterior pancreas and splenic vein, the method of sealing the transected edge of the pancreas (stapler vs. sutures), whether to use of fibrin glue sealant and whether to leave a drain. The method of sealing the transected edge does not appear to influence the formation of postoperative pancreatic fistulas (7).
Neoplasia
Solid pseudopapillary neoplasm
In 2003 a group in France reported on a laparoscopic spleen preserving distal pancreatectomy for a solid pseudopapillary neoplasm (Frantz’s tumor). The report highlights the fact that this was felt to be cutting edge for the time, stating, “Although the role of laparoscopy in surgery of the pancreas is still controversial” it can still “be done safely, within a reasonable operative time, in children.” (8). Since then, there have been a number of case reports describing the success of this technique for pediatric patients with solid pseudopapillary neoplasms (9-14). There has also been a report of a successfully completed robotic-assisted, spleen-preserving, distal pancreatectomy for solid pseudopapillary neoplasm in a child (15). Technical details highlighted from these case series include using a split leg table for larger patients, creating a wide window through the gastrocolic ligament with elevation of the stomach, and dissection along the inferior border of the pancreas to expose the splenic vessels (9,16). Transection of the pancreas may be performed using an endoscopic linear stapler. If the lesion is located more proximally in the gland the pancreas may be divided with mono- and bipolar cautery, then over sewn with 5-0 PDS suture to accommodate for the thickness of the gland (11).
Pancreatic neuroendocrine tumor (pNET)
Insulinomas are the most common functional pNET causing hypoglycemia (17). Most are sporadic, solitary and benign. These factors make them favorable for the minimally invasive approach since they are amenable to parenchyma-sparing techniques such as enucleation (17). An important caveat to this is in the case of multiple endocrine neoplasia type 1 where multifocal disease is more common, oftentimes requiring distal pancreatectomy. Su et al. performed a systematic review of adult patients undergoing laparoscopic versus open pancreatectomy for insulinomas and found that there was no statistically significant difference between the groups with regard to post-operative morbidity including pancreatic fistula, abscess formation, post-operative hemorrhage and reoperation (18). In this subset of patients post-operative development of diabetes mellitus is significant ranging from 12–56% (19). There is a paucity of data detailing the incidence of post-operative diabetes in children following distal pancreatectomy.
Splenic preservation
It is well known that the spleen plays an important role in immunologic function, especially in children. Therefore, with the advancement of minimally invasive techniques for distal pancreatic resection, ensuring splenic preservation is of paramount importance. The magnification imparted by the minimally invasive technique may aid in dissection of the splenic artery and vein off of the pancreatic parenchyma, however this remains a technically challenging component of the procedure. Strategies aimed at assisting in splenic preservation include straightening the splenic artery and vein to improve visualization during the dissection (20). Additionally, early identification of the vessels and medial to lateral dissection may be of benefit (14).
Subtotal pancreatectomy
Hyperinsulinism
Subtotal pancreatectomy is primarily reserved for cases of congenital hyperinsulinemia. Without appropriate treatment, congenital hyperinsulinemia causes persistent hypoglycemia that can lead to irreversible neurologic damage. While clinically identical, congenital hyperinsulinemia may manifest as diffuse or focal disease, which significantly changes the operative approach. Focal lesions amenable to treatment with partial pancreatectomy may be determined using a combination of genetic testing and 18-fluorodopa PET/CT imaging. The most robust report of surgical intervention for congenital hyperinsulinemia was of 500 patients who underwent pancreatectomy at Children’s Hospital of Philadelphia in 2019 (21). However, all of these operations were performed using the open approach. As early as 2001, Blakely reported use of a laparoscopic approach to the initial operation for hyperinsulinism (22). The operation, as described, is likely a 75% resection and proved inadequate due to continued hypoglycemia. However, at laparotomy 1 week later no adhesions were found and the completion pancreatectomy feasible (22). There have been a number of additional descriptions of the laparoscopic approach to near total pancreatectomy (23-25). Pierro et al. describes the laparoscopic technique for subtotal pancreatectomy in children with congenital hyperinsulinemia. Technical pearls include the use of a Nathanson retractor to elevate the stomach, a stay suture in the tail of the pancreas to assist with medial retraction and the use of a 3-mm hook cautery on high coagulation settings to divide the short vessels between the splenic vessels and the pancreas (26). The tail of the pancreas is first removed and sent for frozen section pathological review to confirm the diagnosis prior to proceeding with the remaining resection. Once confirmed, the head and uncinate process are removed leaving a rim of pancreatic parenchyma near the medial border of the duodenum preserving the common bile duct (26).
Enucleation
Enucleation of solitary, benign tumors may reduce the morbidity associated with more extensive pancreatic resections. This technique may be applied with cases of focal hyperinsulinemia, pNETs and small benign lesions that are remote from the main pancreatic duct (17,27). These tumors must be superficial, size less than 2 cm and at least 2 mm from the main pancreatic duct (28). This technique may shorten operative time, decrease blood loss and reduce post-operative pancreatic insufficiency, though robust data regarding these outcomes in children is currently lacking (28). Intraoperative ultrasound is helpful to delineate the relationship between the mass and vascular structures such as the portal vein and superior mesenteric vessels (29).
Lateral pancreaticojejunostomy (Puestow)
Pancreas divisum
One of the most common anatomical variants that leads to recurrent, chronic pancreatitis is pancreas divisum. This occurs when there is incomplete fusion of the dorsal and ventral anlage of the pancreas during fetal development. The result is drainage of the two regions independently into the duodenum. Common features in pancreas divisum include stenosis (typically at the ampulla, but potentially at any branch point within the ductal system) and ectasia. This problem should be considered in any child who has a repeat bout of pancreatitis with no evidence of gallstone disease, though the diagnosis is elusive and not a top contender for consideration in most children with abdominal pain. Neblett et al. describe a single institution series of 130 children with acute, chronic, or relapsing pancreatitis (30). Of these, only 10 were attributed to pancreas divisum. The infrequency of the problem makes diagnosis and comprehensive study difficult. In their study, the average time between onset of symptoms and diagnostic ERCP was almost 6 years (30).
Diagnosis of pancreas divisum is secured with MRCP or ERCP, with the advantage of ERCP being the potential for a definitive, curative procedure performed concurrently. Treatment should be performed in a stepwise fashion, starting with the minimal intervention needed to achieve relief. This typically comes in the form of a sphincterotomy and stenting of the minor papilla, performed by an interventional gastroenterologist during ERCP. Re-stenosis of the minor papilla after removal of the stent is frequent; however, resolution of symptoms following stenting can be regarded as a predictor of success with surgical sphincteroplasty (31). If the minor papilla cannot be cannulated, a surgical sphincteroplasty can be performed. No descriptions of this procedure performed laparoscopically in children exist in the literature to date, likely because of the technical difficulty required to open the duodenum, isolate the papilla, and perform an effective sphincteroplasty. Finally, for patients with failed attempt or no improvement after sphincterotomy or sphincteroplasty, longitudinal pancreaticojejunostomy (Puestow procedure) may prove useful (32).
Description of longitudinal pancreaticojejunostomy using a minimally invasive approach in pediatric patients is limited. The first report in a child was in 2011 by Meehan et al. using a robotic technique (33). Later, in 2012, Zhang et al. described four pediatric patients who successfully underwent laparoscopic side-to-side Roux-Y pancreaticojejunostomy (34). Among the four patients, none had a pancreatic leak, pancreatitis or anastomotic stricture and the length of stay ranged from 4–6 days. Most recently, in 2018 Shah et al. reported two cases of laparoscopic pancreaticojejunostomy for chronic pancreatitis (35). While the second case required conversion to open, the authors concluded that the approach was safe and feasible.
Conclusions
As minimally invasive techniques evolve to become the standard of care among pediatric patients, its use in pancreatic surgery must be carefully examined. Drawing meaningful conclusions from limited pediatric data makes this especially challenging. Though laparoscopic pancreas surgery requires advanced technical abilities, many reports demonstrate its safety and efficacy in a variety of clinical conditions.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Translational Gastroenterology and Hepatology for the series “Current Topics in Pediatric General Surgery”. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at http://dx.doi.org/10.21037/tgh-20-220
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tgh-20-220). The series “Current Topics in Pediatric General Surgery” was commissioned by the editorial office without any funding or sponsorship. Dr. MSC served as the unpaid Guest Editor of the series. Dr. MSC reports personal fees from Bolder Surgical, outside the submitted work. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Yoder SM, Rothenberg S, Tsao K, et al. Laparoscopic treatment of pancreatic pseudocysts in children. J Laparoendosc Adv Surg Tech A 2009;19:S37-40. [Crossref] [PubMed]
- Mattix KD, Tataria M, Holmes J, et al. Pediatric pancreatic trauma: predictors of nonoperative management failure and associated outcomes. J Pediatr Surg 2007;42:340-4. [Crossref] [PubMed]
- Rosenfeld EH, Vogel AM, Jafri M, et al. Management and outcomes of peripancreatic fluid collections and pseudocysts following non-operative management of pancreatic injuries in children. Pediatr Surg Int 2019;35:861-7. [Crossref] [PubMed]
- Iqbal CW, Levy SM, Tsao K, et al. Laparoscopic versus open distal pancreatectomy in the management of traumatic pancreatic disruption. J Laparoendosc Adv Surg Tech A 2012;22:595-8. [Crossref] [PubMed]
- Takishima T, Sugimoto K, Asari Y, et al. Characteristics of pancreatic injury in children: a comparison with such injury in adults. J Pediatr Surg 1996;31:896-900. [Crossref] [PubMed]
- Alemayehu H, Clifton M, Santore M, et al. Minimally invasive surgery for pediatric trauma-a multicenter review. J Laparoendosc Adv Surg Tech A 2015;25:243-7. [Crossref] [PubMed]
- Reynolds EM, Curnow AJ. Laparoscopic distal pancreatectomy for traumatic pancreatic transection. J Pediatr Surg 2003;38:E7-9. [Crossref] [PubMed]
- Carricaburu E, Enezian G, Bonnard A, et al. Laparoscopic distal pancreatectomy for Frantz's tumor in a child. Surg Endosc 2003;17:2028-31. [Crossref] [PubMed]
- Melotti G, Cavallini A, Butturini G, et al. Laparoscopic Distal Pancreatectomy in Children: Case Report and Review of the Literature. Ann Surg Oncol 2007;14:1065-9. [Crossref] [PubMed]
- Fais PO, Carricaburu E, Sarnacki S, et al. Is laparoscopic management suitable for solid pseudo-papillary tumors of the pancreas? Pediatr Surg Int 2009;25:617-21. [Crossref] [PubMed]
- Sokolov YY, Stonogin SV, Donskoy DV, et al. Laparoscopic pancreatic resections for solid pseudopapillary tumor in children. Eur J Pediatr Surg 2009;19:399-401. [Crossref] [PubMed]
- Uchida H, Goto C, Kishimoto H, et al. Laparoscopic spleen-preserving distal pancreatectomy for solid pseudopapillary tumor with conservation of splenic vessels in a child. J Pediatr Surg 2010;45:1525-9. [Crossref] [PubMed]
- Petrosyan M, Franklin AL, Jackson HT, et al. Solid pancreatic pseudopapillary tumor managed laparoscopically in adolescents: a case series and review of the literature. J Laparoendosc Adv Surg Tech A 2014;24:440-4. [Crossref] [PubMed]
- Kovler ML, Beckman RM, Goldstein SD, et al. Laparoscopic Spleen-Preserving Distal Pancreatectomy for Solid Pseudopapillary Neoplasm in Adolescents. J Laparoendosc Adv Surg Tech A 2019;29:1372-7. [Crossref] [PubMed]
- Lalli R. Robotic-assisted, spleen-preserving distal pancreatectomy for a solid pseudopapillary tumour in a pediatric patient: a case report and review of the literature. J Robot Surg 2019;13:325-9. [Crossref] [PubMed]
- Cavallini A, Butturini G, Daskalaki D, et al. Laparoscopic Pancreatectomy for Solid Pseudo-Papillary Tumors of the Pancreas is a Suitable Technique; Our Experience with Long-Term Follow-up and Review of the Literature. Ann Surg Oncol 2011;18:352-7. [Crossref] [PubMed]
- Shirota T, Nagakawa Y, Sahara Y, et al. Surgical resection of neuroendocrine tumors of the pancreas (pNETs) by minimally invasive surgery: the laparoscopic approach. Gland Surg 2018;7:12-9. [Crossref] [PubMed]
- Su AP, Ke NW, Zhang Y, et al. Is laparoscopic approach for pancreatic insulinomas safe? Results of a systematic review and meta-analysis. J Surg Res 2014;186:126-34. [Crossref] [PubMed]
- Esposito C, de Lagausie P, Escolino M, et al. Laparoscopic Resection of Pancreatic Tumors in Children: Results of a Multicentric Survey. J Laparoendosc Adv Surg Tech A 2017;27:533-8. [Crossref] [PubMed]
- Nagakawa Y, Sahara Y, Hosokawa Y, et al. The Straightened Splenic Vessels Method Improves Surgical Outcomes of Laparoscopic Distal Pancreatectomy. Dig Surg 2017;34:289-97. [Crossref] [PubMed]
- Adzick NS, De Leon DD, States LJ, et al. Surgical treatment of congenital hyperinsulinism: Results from 500 pancreatectomies in neonates and children. J Pediatr Surg 2019;54:27-32. [Crossref] [PubMed]
- Blakely ML, Lobe TE, Cohen J, et al. Laparoscopic pancreatectomy for persistent hyperinsulinemic hypoglycemia of infancy. Surg Endosc 2001;15:897-8. [Crossref] [PubMed]
- Bax KN, van der Zee DC. The laparoscopic approach toward hyperinsulinism in children. Semin Pediatr Surg 2007;16:245-51. [Crossref] [PubMed]
- Al-Shanafey S. Laparoscopic vs open pancreatectomy for persistent hyperinsulinemic hypoglycemia of infancy. J Pediatr Surg 2009;44:957-61. [Crossref] [PubMed]
- Zhang JS, Li L, Cheng W. Single incision laparoscopic 90% pancreatectomy for the treatment of persistent hyperinsulinemic hypoglycemia of infancy. Pediatr Surg Int 2016;32:1003-7. [Crossref] [PubMed]
- Pierro A, Nah SA. Surgical management of congenital hyperinsulinism of infancy. Semin Pediatr Surg 2011;20:50-3. [Crossref] [PubMed]
- Liang M, Jiang J, Dai H, et al. Robotic enucleation for pediatric insulinoma with MEN1 syndrome: a case report and literature review. BMC Surg 2018;18:44. [Crossref] [PubMed]
- Liu R, Wakabayashi G, Palanivelu C, et al. International consensus statement on robotic pancreatic surgery. Hepatobiliary Surg Nutr 2019;8:345-60. [Crossref] [PubMed]
- Fisher JC, Kuenzler KA, Bodenstein L, et al. Central pancreatectomy with pancreaticogastrostomy in children. J Pediatr Surg 2007;42:740-6. [Crossref] [PubMed]
- Neblett WW, O'Neill JA. Surgical management of recurrent pancreatitis in children with pancreas divisum. Ann Surg 2000;231:899-908. [Crossref] [PubMed]
- Tringali A, Voiosu T, Schepis T, et al. Pancreas divisum and recurrent pancreatitis: long-term results of minor papilla sphincterotomy. Scand J Gastroenterol 2019;54:359-64. [Crossref] [PubMed]
- Hodgman E, Megison S, Murphy J. Puestow Procedure for the Management of Pediatric Chronic Pancreatitis. Eur J Pediatr Surg 2019;29:153-8. [Crossref] [PubMed]
- Meehan JJ, Sawin R. Robotic lateral pancreaticojejunostomy (Puestow). J Pediatr Surg 2011;46:e5-8. [Crossref] [PubMed]
- Zhang JS, Li L, Liu SL, et al. Laparoscopic pancreaticojejunostomy for pancreatic ductal dilatation in children. J Pediatr Surg 2012;47:2349-52. [Crossref] [PubMed]
- Shah AA, Petrosyan M, Kane TD. Lateral Pancreaticojejunostomy for Chronic Pancreatitis and Pancreatic Ductal Dilation in Children. J Laparoendosc Adv Surg Tech A 2018;28:1397-402. [Crossref] [PubMed]
Cite this article as: Richards MK, Clifton MS. Minimally invasive surgery of the pancreas: a narrative review of current practice. Transl Gastroenterol Hepatol 2021;6:38.


