
A retrospective analysis of pancreas operations in children
Introduction
Operative pancreatic interventions are relatively rare in the pediatric population (1-3). There are a variety of indications which may require pancreas surgery in children. These include malignancy, trauma, and chronic pancreatitis (4-7). The literature reviewing pancreas procedures in children is growing, yet remains sparse with regards to a comprehensive understanding of how particular pancreas operations are applied across a range of childhood pancreatic disorders. Data regarding the indications for pancreatic operations and the ensuing outcomes is needed in this population in order to better inform clinical management and direct future studies. This report reviews all pancreas operations performed in children at a single institution. We desired to demonstrate the indications for these procedures and hypothesized that these operations are safe and effective in the pediatric population. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/tgh-20-260).
Methods
Database and case identification
This is a retrospective single-institution observational cohort study. After institutional review board (IRB) approval, the electronic medical record was reviewed for all children ages 0 to 18 years who underwent the following operations: distal pancreatectomy, pancreaticoduodenectomy (Whipple), lateral pancreaticojejunostomy (Puestow), central pancreatectomy, and total pancreatectomy. All cases were included to avoid sampling biases. Our institution does not perform total pancreatectomy for islet auto-transplantation. Cases were identified based upon current procedural technology® (CPT) codes corresponding with the listed procedures. No children were excluded. Given the retrospective nature of the study, the requirement for informed consent was waived by the IRB. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the institutional review board of the University of Texas Southwestern Medical Center and Children’s Health (IRB # STU 022015-094).
Outcomes and analysis
Following case identification, charts were reviewed in a standardized fashion to obtain the following data: demographics, operative indications, procedure duration, estimated blood loss (EBL), length of hospital stay (LOS), presence of intensive care unit (ICU) stay and duration, pathologic diagnosis, complications, readmissions, and mortality. Follow-up was defined by outpatient postoperative clinic visits and recorded in months. Data was collected via standardized form to reduce bias during abstraction. There was no missing data. Descriptive calculations included frequencies for categorical variables and means and ranges for numerical variables. All statistical analyses were completed with SPSS 25 (IBM, Armonk, NY, USA).
Results
A total of 46 patients underwent 47 pancreas resections during the study period. Table 1 summarizes patient data by type of pancreas resection, including indications for surgery and demographics. Pancreatic mass was the most common indication for resection (n=28, 60%), followed by traumatic injury (n=10, 21%) and chronic pancreatitis (n=8, 17%). With regards to operative intervention for pancreas trauma, there were 174 total cases of pancreas trauma during the study period, including contusion and laceration. Therefore, approximately 6% of pancreas trauma patients required operative intervention at our institution. There were 28 (60%) distal pancreatectomies, 1 (2%) central and 1 (2%) total pancreatectomies, 9 (20%) Whipple, and 8 (17%) Puestow procedures performed. Two distal pancreatectomies were performed in the same patient for recurrent desmoid tumor. This was the only recurrent tumor that required reoperation; other malignancies including pancreatoblastoma achieved complete excision. There was a female predominance across all operations and age at surgery ranged from 5 months to 18 years. Indications for each operation are listed in the table. Across all operations, the most common pathology was solid pseudopapillary tumor (SPT) (n=14, 31%), followed by traumatic injury (n=10, 22%) and chronic pancreatitis (n=7, 16%). There were no patients treated for congenital hyperinsulinism at our institution.
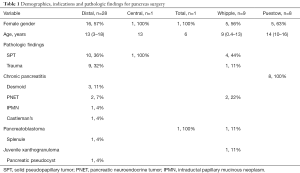
Full table
Intraoperative outcomes are shown in Table 2. The average length of procedure was 4.5 hours (range, 1.9–11.1 hours) with an EBL of 210 mL (range, 1–1,500 mL). Four (9%) patients required intraoperative transfusion. Twelve (26%) patients were admitted to the ICU postoperatively for an average stay of 3.5 days (range, 1–13 days). Postoperatively, 11 (23%) patients required total parental nutrition. Average total LOS was 9.8 days (range, 1–62 days). Drains were placed intraoperatively at the index operation in 29 (62%) of the cases; only one patient required interventional drainage postoperatively.
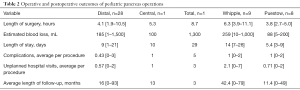
Full table
The overall complication rate was 0.55 (range, 0–3) complications per procedure, including 4 pancreatic leaks; 19 patients (40%) had any complication postoperatively. Therefore, 60% of cases experienced no postoperative complications. All complications are listed in Table 3. The most common complications were ileus and pancreatic leak. Other complications included wound infection and dehiscence, ileus, pulmonary edema, intra-abdominal infection requiring drainage, acute pancreatitis, pneumonia, seizure, hemorrhage and diabetes. Ileus was defined by inability to tolerate oral intake for >3 days postoperatively, or need for parenteral nutrition and/or nasogastric drainage with inability to tolerate oral intake. The overall unexpected hospital visit rate (emergency department and readmissions) was 0.76 (range, 0–6) visits per patient. Average length of follow up with 20 months (range, 0–93 months) (Table 2). There were no mortalities.
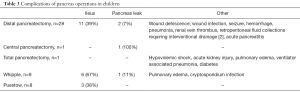
Full table
Whipple
Nine patients underwent a Whipple procedure. The most common indication was SPT and all were performed open. The average LOS was 14 days, with 6 patients admitted post operatively to the ICU for an average of 2.5 days. The average length of surgery was 6.3 hours with 259 mL EBL (Table 2).
Distal pancreatectomy
Twenty-eight patients underwent a distal pancreatectomy. The most common indications were SPT and trauma. Eight patients had laparoscopy or robot-assisted laparoscopy and the remaining 19 had an open procedure. The LOS (11.16 vs. 5.25 days, P=0.22), EBL (240 vs. 59 mL, P=0.25), length of surgery (3.9 vs. 4.2 hours, P=0.82), and ICU admission (32% vs. 12.5%, Chi squared P=0.63) were not statistically different between the open and laparoscopic groups.
Puestow
All 8 patients undergoing a Puestow had chronic pancreatitis, and they were performed open with a Roux-en-Y pancreaticojejunostomy. Indications for this procedure included recurrent pancreatitis with dilated pancreas duct as noted on preoperative imaging. Average LOS (5 days), length of surgery (3.7 hours), EBL (86 mL) are listed in Table 2. No patients required an ICU admission. Three patients developed postoperative pancreatitis during the follow-up period.
Discussion
We present a comprehensive report of all pancreatic operations performed in children at a single institution. These data provide granular detail regarding pathologic indications for pediatric pancreas surgery, along with outcomes and complications associated with these operations. This information is important to inform management and counseling of pediatric pancreas surgery patients who will inevitably present to pediatric surgeons, many of whom may manage these patients less frequently than others. These procedures are rare in children, and do carry an associated complication rate.
Patient cohort
Similar age ranges and female predominance of pancreas operations are described in other retrospective reviews of pediatric pancreas operations at other institutions (1,8). With regards to resection of pancreatic masses/tumors, the most common pathology noted across all patients was SPT. Previous studies have identified the preponderance of this pathology in pediatric pancreas operations (3,9,10). On the other hand, we only operated on a total of two patients for pancreatic neuroendocrine tumor, while other case series describe this histopathology at a higher rate (3). With regards to malignant pancreas tumors, we present two patients with pancreatoblastoma, but no ductal adenocarcinoma or neuroblastoma in our experience.
Operative procedures
The most common operative procedure in our series was distal pancreatectomy [27], followed by Whipple [9] and Puestow [7]. The type and extent of the resection was dictated by the injury, tumor, or pattern of duct dilation for chronic pancreatitis, akin to other studies. We align with previous studies that surgical management of pancreatic malignancy remains the mainstay of treatment for best long-term outcomes (1,7,11,12). We did not perform any duodenal sparing operations during resections of the pancreas head, which has shown success at other centers (13). Similarly, surgical management of pancreatic trauma was guided by extent and location of duct injury, as well as timing relative to onset of injury (14-16). We did not include internal drainage for post-traumatic pseudocyst as it did not require resection of the pancreas. All patients with chronic pancreatitis underwent a Puestow procedure.
Generally, the majority of the operations were done open. Specifically, for the patients undergoing the Whipple procedure, we performed a pylorus sparing Whipple in 6 of the 9 patients (67%). Eight of 27 distal pancreatectomies were performed by laparoscopy or robot-assisted laparoscopy (30%). Previous studies have that open and laparoscopic approaches are equivalent in the operative management of pediatric pancreas trauma when distal pancreatectomy is the indicated procedure (17). Given the retrospective nature of our study we anticipate that the lack of statistical difference between the open and laparoscopic distal pancreatectomy is owed to patient selection and surgeon preference.
Limitations and future directions
Our study is a single-institution retrospective review, and as such, limited by the inherent biases of the design. However, we were able to accrue 46 patients during our study period with a robust follow up of 20 months on average. Although our patient cohort is smaller in volume than a database study, our data is more granular. Additionally, we present the case variety that represent what many pediatric surgeons have in their own practice, with trauma, malignancy, and chronic pancreatitis. We believe our data will be generalizable to the practicing pediatric general surgeon. However, future studies should aim to pool data from multiple institutions in order to improve statistical power and reduce bias. Additionally, we did not implement postoperative enhanced recovery protocols during the study period. Doing so could for allow standardization of postoperative course and improved outcomes and is an area for future quality improvement. Multi-institutional data will improve generalizability and overall understanding of pancreas surgery in children.
Conclusions
Our series describes a variety of pathology for which pediatric surgeons may be called upon to perform pancreatic surgeries, with demonstration of safety and feasibility across different anatomic resections. Although we were limited by the single institution nature of our experience, our data show clear indications for pancreatic surgery in this population. Knowledge of potential outcomes and complications may assist in patient and family counseling.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Eduardo Perez, Samir Pandya, and Matthew S. Clifton) for the series “Current Topics in Pediatric General Surgery” published in Translational Gastroenterology and Hepatology. The article has undergone external peer review.
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/tgh-20-260
Data Sharing Statement: Available at http://dx.doi.org/10.21037/tgh-20-260
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tgh-20-260). The series “Current Topics in Pediatric General Surgery” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the institutional review board of the University of Texas Southwestern Medical Center and Children’s Health (IRB # STU 022015-094). The requirement for informed consent was waived by the IRB given the retrospective nature of this study. Patient personal data was kept secure and protected.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Cheng H, Yang S, Ren Q, et al. Pancreatectomies for Pediatric Pancreatic Tumors: A Single Institute Experience from 2007 to 2018. J Pediatr Surg 2019;S0022-3468(19)30591-3.
- Picado O, Ferrantella A, Zabalo C, et al. Treatment patterns and outcomes for pancreatic tumors in children: an analysis of the National Cancer Database. Pediatr Surg Int 2020;36:357-63. [Crossref] [PubMed]
- Sacco Casamassima MG, Gause CD, Goldstein SD, et al. Pancreatic surgery for tumors in children and adolescents. Pediatr Surg Int 2016;32:779-88. [Crossref] [PubMed]
- Crombleholme TM, deLorimier AA, Way LW, et al. The modified Puestow procedure for chronic relapsing pancreatitis in children. J Pediatr Surg 1990;25:749-54. [Crossref] [PubMed]
- Paul MD, Mooney DP. The management of pancreatic injuries in children: operate or observe. J Pediatr Surg 2011;46:1140-3. [Crossref] [PubMed]
- Laje P, Adzick NS. Modified Puestow procedure for the management of chronic pancreatitis in children. J Pediatr Surg 2013;48:2271-5. [Crossref] [PubMed]
- Lindholm EB, Alkattan AK, Abramson SJ, et al. Pancreaticoduodenectomy for pediatric and adolescent pancreatic malignancy: A single-center retrospective analysis. J Pediatr Surg 2017;52:299-303. [Crossref] [PubMed]
- Muller CO, Guerin F, Goldzmidt D, et al. Pancreatic resections for solid or cystic pancreatic masses in children. J Pediatr Gastroenterol Nutr 2012;54:369-73. [Crossref] [PubMed]
- Zampieri N, Schiavo N, Capelli P, et al. Pseudopapillary tumor in pediatric age: clinical and surgical management. Pediatr Surg Int 2011;27:1271-5. [Crossref] [PubMed]
- van den Akker M, Angelini P, Taylor G, et al. Malignant pancreatic tumors in children: a single-institution series. J Pediatr Surg 2012;47:681-7. [Crossref] [PubMed]
- Mansfield SA, Mahida JB, Dillhoff M, et al. Pancreaticoduodenectomy outcomes in the pediatric, adolescent, and young adult population. J Surg Res 2016;204:232-6. [Crossref] [PubMed]
- Rojas Y, Warneke CL, Dhamne CA, et al. Primary malignant pancreatic neoplasms in children and adolescents: a 20 year experience. J Pediatr Surg 2012;47:2199-204. [Crossref] [PubMed]
- Snajdauf J, Rygl M, Petru O, et al. Indications and outcomes of duodenum-preserving resection of the pancreatic head in children. Pediatr Surg Int 2019;35:449-55. [Crossref] [PubMed]
- Meier DE, Coln CD, Hicks BA, et al. Early operation in children with pancreas transection. J Pediatr Surg 2001;36:341-4. [Crossref] [PubMed]
- Naik-Mathuria BJ, Rosenfeld EH, Gosain A, et al. Proposed clinical pathway for nonoperative management of high-grade pediatric pancreatic injuries based on a multicenter analysis: A pediatric trauma society collaborative. J Trauma Acute Care Surg 2017;83:589-96. [Crossref] [PubMed]
- Rosenfeld EH, Vogel A, Russell RT, et al. Comparison of diagnostic imaging modalities for the evaluation of pancreatic duct injury in children: a multi-institutional analysis from the Pancreatic Trauma Study Group. Pediatr Surg Int 2018;34:961-6. [Crossref] [PubMed]
- Iqbal CW, Levy SM, Tsao K, et al. Laparoscopic versus open distal pancreatectomy in the management of traumatic pancreatic disruption. J Laparoendosc Adv Surg Tech A 2012;22:595-8. [Crossref] [PubMed]
Cite this article as: Jones RE, Zagory JA, Tatum M, Tsui WS, Murphy J. A retrospective analysis of pancreas operations in children. Transl Gastroenterol Hepatol 2021;6:39.


