
Prevalence of hepatitis B virus among children of HBsAg-positive mothers in Hebron district, Palestine
Introduction
Hepatitis B virus (HBV) infection is a major public health problem in the Middle East. It has been estimated that around 240 million individuals suffer from this infection in low- and middle-income countries, with an intermediate or high endemic of HBV infection (1,2). This infection is likely to cause liver cirrhosis, chronic hepatitis, and hepatocellular carcinoma. The remainder persists chronic infection in the carrier individuals; although, majority of the cases of these infections are self-limiting (1). The HBV acquired via mother-to-child transmission is the major cause of transmission among the infants and children in the endemic areas (3). The children are at increased risk from long-term interpersonal contact with the infected mother, even if the children do not present any symptoms of HBV infection (4).
West Bank in Palestine is considered an intermediate endemic area of hepatitis B (5). HBV is a special problem for pregnant woman, who are likely to face the risk of hepatitis herself and also pass it to her baby via vertical transmission (6). Previous studies have shown that the outcome of HBV infection is documented in relation to the time of exposure because the morbidity and mortality rates correspond to early neonatal exposure (7,8). About 40% of the infants delivered by infected mothers are likely to develop HBV infections in the absence of post exposure prophylaxis (9). There is increased occurrence of mother to child transmission of hepatitis B, despite of various intervention of vaccinations and immunoglobulins.
The hepatitis B surface antigen (HBsAg) mothers with HBV DNA levels greater than or equal to 106 copies per milliliter are more likely to transmit the virus to their infants; although, there is HBsAg positivity. It has been shown that increased maternal load is considered as an important risk factor that favors the transmission of HBV (10). There is a chance of 5–10 percent failure rate even, when the women have access to birth dose vaccine of HBV and hepatitis B immunoglobulin (11). However, in such conditions, risk of transmission can be reduced through antiviral therapy during pregnancy. The factors affecting the percentage of seropositivity for HBsAg in HBsAg-carrier mothers include; age of gestation, HBV genotype/subgenotype, and HBV genotype/subgenotype.
The age of patient at acquisition of the virus is considered as the determining factor for the progression of acute condition to chronic lifelong carrier stage. The children are likely to develop chronic infection if they have acquired the infection perinatally of within 6 years of age (12). The risk of vertical transmission can be minimized by vaccination. Both hepatitis B active vaccine and hepatitis B immunoglobulin are needed for preventing HBV infection in infants born to HBsAg-positive women (13). It is difficult to analyze that majority of the infants (90%) infected perinatally with HBV are followed by a chronic course of infection. Therefore, the present study aims to determine the prevalence of hepatitis B infection among children born to HBsAg-positive mothers in Hebron district and the socio-demographic correlations with its prevalence.
Methods
Study design and setting
The study was conducted during the year 2017 in Hebron district that is situated 40 km south from Jerusalem. It is the largest district in the West Bank in terms of size and population of 729,000 (14) with large distribution in rural areas. Two hospitals situated within the Hebron district, having a routine practice of testing pregnant women for HBV at the time of admission for delivery were selected for collaboration in the study.
Study participants
Blood samples of women and their children were screened by enzyme-linked immunosorbent assay (ELISA) for HBsAg. The study enrolled and tested 125 HBsAg-positive women and their children in the study. The overall number of HBsAg-positive children born to HBsAg-positive mothers were found to be 42 out of 386 tested children (10.9%). It was made sure that participated woman in study had positive HBsAg when they were pregnant. The women presented with HBsAg positive received an information letter, in which they were explained about the purpose of the study and the confidential of the results. A consent form was signed by all the included participants before commencing the study. It was also made sure that the newborn recruited in the study were given a protective immunoglobulin in the first 24 hours of birth.
Data collection
For those who agreed, a multiple choice-based questionnaire was completed by the help of a nurse via patient interview to ensure proper data collection and prevent any misunderstanding. The questionnaire contained socio-demographic questions, including age, place of residence, occupation, level of education, as well as questions related to expected route of exposure to the virus and the type of vaccination, they provided to their previous born children (15). Blood samples were collected from mothers’ children upon oral consent of participation. For HBsAg determination, Axsym HBsAg version 2.0 Kit (Abbott, Germany) was used.
Data analysis
The data was collected, summarized, tabulated, and analyzed using the statistical package for social sciences (SPSS) V.15 software. The results were explained based on the descriptive statistics that included frequencies and percentages.
Ethical considerations
The study has been approved by the international review board (IRB) of Ethics Committee Herbon University, Palestine under the code SR/122/2016.
Results
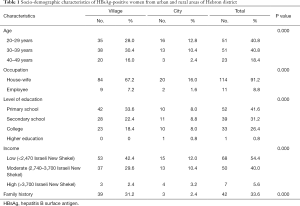
The results showed that HBsAg-positive children were 42 (10.9%). The positive children belonged to 15 families out of the 125 studied families. Moreover, these children seem to be infected by vertical transmission route. These children belonged to families living in villages with low to moderate income (P value =0.000). About 33.6% of HBsAg-positive women had family history of HBV infection, either their mothers or some family members were carriers (P value =0.000). Table 1 has shown that 61.6% of HBsAg-positive women had no family history with unknown route of transmission; although, 23.1% of HBsAg-positive women (19 from villages and 11 from the city) suspected in dental clinics. They were infected with hepatitis B after repeated visits to private dental clinics.
Full table
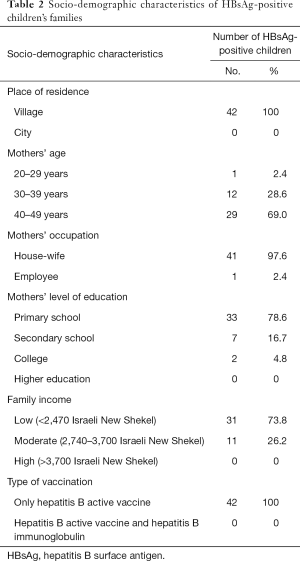
In the present study, 42 children were found to be HBsAg-positive, reflecting the fact that these children belong to low to moderate income families. These families knew that the mother was carrier of hepatitis B, but they were not able to provide hepatitis B immunoglobulin to their newborns. Out of 386 children born to HBsAg-positive mothers only 251 (65.0%) received both vaccines (hepatitis B active vaccine and Hepatitis B immunoglobulin). Whereas, 135 (35.0%) of children born to HBsAg-positive mothers received only hepatitis B active vaccine without hepatitis B immunoglobulin. The occurrence of HBsAg among children increased with mother’s age (old mothers had more HBsAg positive children) and was inversely proportional with mother’s level of education (Table 2).
Full table
Discussion
The incidence rate of hepatitis B cases per 100,000 dropped from (11-15) in the years 1990–1994 to (0.56) in the year 2015 (16), after the implementation of hepatitis B immunization (active vaccine) in Palestine in 1993. The newborn recruited in the study were given a protective immunoglobulin in the first 24 hours of birth. However, the previous children of some of these families had not given any protective immunoglobulin due to economic obstacles and unawareness of this infection. In the present study, 42 children were found to be HBsAg-positive, reflecting the fact that all these children belonged to low to moderate income families. Moreover, not all the hospitals and birth centers in the studied area test women for hepatitis B before labor and delivery, which may increase the possibility of vertical transmission of HBV. Some of the mothers in this study admitted that they only knew about their hepatitis B infection after they transmitted the infection to their children.
Hepatitis B is a blood-borne and sexually transmitted disease, which clearly explains its prevalence among women with family history of hepatitis B infection (33.6%). The present study has determined the prevalence of hepatitis B among children born to HBsAg positive women in Hebron district/Palestine. At the same time, the higher percentage of this infection was seen in rural areas, which reflects the ignorance and lack of awareness in these areas in comparison with urban areas. The majority of HBsAg-positive women were unaware about the source of infection; however, many of them (23.1%) suspected in dental clinics; they were infected after several visits to private dental clinics in their areas. Hepatitis B is a well-recognized blood-borne infection and it can be transmitted through clinics if there was no adherence to recommended infection control practices (17). The role of private clinics in transmitting HBV needs more investigation and can be considered an important risk factor in absence of routine surveillance by the ministry of health.
Hepatitis B active vaccination had proven to be very effective in protecting infants, but in the case of newborns of HBsAg-positive mothers, immunoglobulin also is needed to protect against vertical transmission (18). HBsAg-positive women can contribute to new cases of HBsAg-positive newborns, who have more possibility to account to chronic carriers in the country. West Bank has an incidence rate of hepatitis B carriers of (23.0) per 100,000 population (16). Providing these newborns with hepatitis B immunoglobulin with complete coverage, should be a strategy for the ministry of health in Palestinian society as part of the preventive services, which are well established practices in many countries across the world (19).
The study focuses on universal screening of all pregnant women for HBV infection in the endemic areas. The results have shown the importance of effective preventive measures among the women at high risk starting from pregnancy to delivery. Previous studies have shown that HBsAg positive mother is at increased risk (10–30%) of delivering a child, who is chronic carrier of HBV (11,20,21). This study showed that not all children who only received active vaccine without immunoglobulin had developed the infection, since the levels of maternal HBV DNA is considered as the most significant risk factor that favors the transmission of hepatitis B in the infants during pregnancy. A similar study conducted by Nelson et al. (22) showed that the risk of transmission of HBV is highest in the case of maternal acquisition of HBV infection, in the third trimester of pregnancy. The association between positive HBsAg mothers with higher HBV DNA viral loads is well-documented with increased chances of mother to child transmission (23).
There is need to sustain the current active vaccination for eliminating hepatitis B vertical transmission, along with the hepatitis B immunoglobulins for all infants of hepatitis B carrier mothers. Results show that 35% of the children born to HBsAg-positive mothers only received hepatitis B active vaccine without immunoglobulin due to unawareness of the infection or due to economic difficulties. The study recommends that infants born to HBsAg positive mothers should receive timely and adequate post-exposure prophylaxis with full coverage from the Ministry of Health. The study results are limited due to a small sample size and focusing only a small endemic area. Moreover, the study has only verified a single route of transmission of HBV infection.
The present study has considered women in Hebron district and assessed the prevalence of hepatitis B among children born to HBsAg positive women. The study findings have shown that majority of the infected children were infected by vertical transmission route and belonged to mothers living in villages with low to moderate income. These findings suggest the need of presenting integrated information and educational programs to prevent and control HBV transmission among this target group. Future studies need to verify the unknown routes of transmission and to reduce the possible risk factors. Moreover, other similar studies from various subsamples of general Palestinian population are required to get clearer understanding of HBV epidemiology in general.
Acknowledgments
The author is very thankful to all the associated personnel in any reference that contributed in/for the purpose of this research.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study has been approved by the international review board (IRB) of Ethics Committee Herbon University, Palestine under the code SR/122/2016.
References
- World Health Organization. Guidelines for the prevention care and treatment of persons with chronic hepatitis B infection. Geneva: World Health Organization, 2015.
- GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;385:117-71. [Crossref] [PubMed]
- Li Z, Hou X, Cao G. Is mother-to-infant transmission the most important factor for persistent HBV infection? Emerg Microbes Infect 2015;4:e30. [Crossref] [PubMed]
- Locarnini S, Hatzakis A, Chen DS, et al. Strategies to control hepatitis B: public policy, epidemiology, vaccine and drugs. J Hepatol 2015;62:S76-86. [Crossref] [PubMed]
- Ministry of Health. PHIC, Health Status in Palestine 2011. 2012.
- Lin CL, Kao JH. Hepatitis B viral factors and clinical outcomes of chronic hepatitis B. J Biomed Sci 2008;15:137-45. [Crossref] [PubMed]
- Shepard CW, Simard EP, Finelli L, et al. Hepatitis B virus infection: epidemiology and vaccination. Epidemiol Rev 2006;28:112-25. [Crossref] [PubMed]
- Han GR, Xu CL, Zhao W, et al. Management of chronic hepatitis B in pregnancy. World J Gastroenterol 2012;18:4517-21. [Crossref] [PubMed]
- Centers for Disease Control and Prevention. Viral hepatitis—hepatitis B perinatal transmission. 2015. Available online: www.cdc.gov/ hepatitis/hbv/perinatalxmtn.htm
- Giles ML, Grace R, Tai A, et al. Prevention of mother-to-child transmission of hepatitis B virus (HBV) during pregnancy and the puerperium: current standards of care. Aust N Z J Obstet Gynaecol 2013;53:231-5. [Crossref] [PubMed]
- Anderson, M. Mother-to-child transmission of hepatitis B in Africa: is elimination feasible? 2015. Retrieved from: http:// www.sacemaquarterly.com/wpcontent/uploads/2015/03/ Andersson-mother-to-child-article1.pdf.
- Seeger C, Mason WS. Molecular biology of hepatitis B virus infection. Virology 2015;479-480:672-86. [Crossref] [PubMed]
- Nelson NP, Easterbrook PJ, McMahon BJ. Epidemiology of hepatitis B virus infection and impact of vaccination on disease. Clin Liver Dis 2016;20:607-28. [Crossref] [PubMed]
- Palestinian Central Bureau of Statistics (PCBS). Population projects. 2017. Available online: http://www.pcbs.gov.ps/site/803/default.aspx
- Nijem KI, Al-Amleh S. Seroprevalence and associated risk factors of toxoplasmosis in pregnant women in Hebron district, Palestine. East Mediterr Health J 2009;15:1278-84. [PubMed]
- Palestinian National Information Center (PHIC). Health annual report. 2016. Available online: https://www.philhealth.gov.ph/about_us/annual_report/ar2016.pdf
- Radcliffe RA, Bixler D, Moorman A, et al. Hepatitis B virus transmissions associated with a portable dental clinic, West Virginia, 2009. J Am Dent Assoc 2013;144:1110-8. [Crossref] [PubMed]
- Kuhail S, el-Khodary R, Ahmed F. Evaluation of the routine hepatitis B immunization programme in Palestine, 1996. East Mediterr Health J 2000;6:864-9. [PubMed]
- Kemper AR, Krist AH, Tseng CW, et al. Challenges in developing U.S. preventive services task force child health recommendations. Am J Prev Med 2018;54:S63-9. [Crossref] [PubMed]
- Cheung KW, Seto MT, Wong SF. Towards complete eradication of hepatitis B infection from perinatal transmission: review of the mechanisms of in utero infection and the use of antiviral treatment during pregnancy. Eur J Obstet Gynecol Reprod Biol 2013;169:17-23. [Crossref] [PubMed]
- Isa MA, Bello HS, Gulani IA, et al. Prevalence of hepatitis B virus infection among children attending Mohammed Shuwa Memorial Hospital, Maidaguri, Borno State, Nigeria. Int J Adv Res Bio Sci 2015;2:128-32.
- Nelson NP, Jamieson DJ, Murphy TV. Prevention of perinatal hepatitis B virus transmission. J Pediatric Infect Dis Soc 2014;3 Suppl 1:S7-12. [Crossref] [PubMed]
- Andersson MI, Rajbhandari R, Kew MC, et al. Mother-to-child transmission of hepatitis B virus in sub-Saharan Africa: time to act. Lancet Glob Health 2015;3:e358-9. [Crossref] [PubMed]
Cite this article as: Al-Amleh S. Prevalence of hepatitis B virus among children of HBsAg-positive mothers in Hebron district, Palestine. Transl Gastroenterol Hepatol 2020;5:34.


