South Coast appendicular mass management (SCAM) survey
Introduction
Acute appendicitis is one of the most common acute surgical conditions. The defense mechanism of the patient’s body may control the acute situation by forming an inflammatory mass (an appendiceal phlegmon) or a confined abscess, often presenting as a palpable, tender mass usually 5 to 7 days following the onset of symptoms (1,2). Mass formation occurs in 2% to 7% of all cases of acute appendicitis (1,2).
The management of appendicular mass is still controversial despite several innovative diagnostic and operative interventions in the field of emergency surgery. Urgent appendicectomy may be technically difficult because of the distorted anatomy and tissue friability. Sometimes the resulting procedure is either ileocecal resection or even a right hemicolectomy because appendicular mass is mimicking a neoplastic growth (3). Conservative management of appendicular mass has been facilitated by improved imaging techniques and image-guided therapeutic intervention with the help of computerized tomography (CT) and ultrasonography (4). Newer antibiotics have also catalyzed nonsurgical treatment (5). Though, the third option of conservative management with interval appendectomy has traditionally remained the gold standard management, necessity of interval appendicectomy has always been questioned as the risk of recurrence is relatively small and increased health burden issue (6). Interestingly, one recent randomized controlled trial (RCT) from Finland showed the alarmingly increased incidence of appendicular neoplasm (overall 20%) following interval appendicectomy in the age group of more than forty years which prompted a premature termination of the study (7).
The ongoing debate in the management plan of appendicular mass has prompted the authors to conduct this study to search the most commonly practiced approach among the senior surgeons in the hospitals at South Coast of England named as South Coast appendicular mass management (SCAM) survey.
Methods
Following the recent publication of a RCT (7) advocating the need of interval appendectomy in patients presenting with appendicular mass due to an alarming incidence of neoplastic lesions on histopathological examination of resected appendix among patients with the age of more than forty years, the idea of SCAM survey was conceived and discussed in the departmental clinical governance meeting. A proforma (Figure 1) was prepared by four consultants and one senior surgical registrar with main headings focusing on “diagnostic criteria”, “initial management pathway”, “intervention radiological drainage”, “discharge criteria”, “follow up investigation”, “interval appendicectomy”, “time interval for interval appendicectomy”, “chase up for histopathology report of the specimen” and “other comments”. We collected the data by e-mailing the proforma to surgical consultants, surgical trainees of registrar grade and staff grade surgeons. Data was also collected by direct phone calls to relevant surgeons, to improve the response rate. The data from completed proforma was transferred to the Microsoft Excel sheet. Data analysis and interpretation were performed by two authors (Muhammad S. Sajid and Kausik Ray).
Results
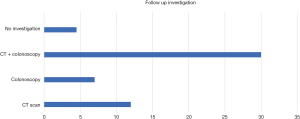
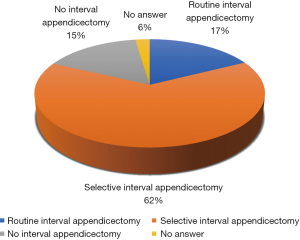
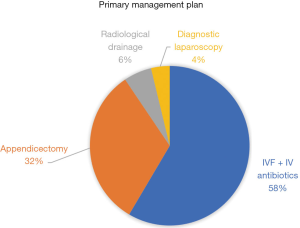
Fifty-three surgeons [22 consultants, 27 senior surgical specialty trainees (ST3–ST8) and 4 staff grade surgeons] completed the proforma. Nineteen out of 53 (36%) participants agreed clinical, hematological and CT based diagnostic criteria at the initial stage whereas 27 surgeons (51%) suggested clinical examination followed by CT scan. For initial management, around 58% participants (31/53) offered intravenous fluids (IVF) and antibiotics (ABTXs) and around 6% (3/53) suggested radiology-assisted drainage in addition to this. Thirty-two percent (17/53) surgeons offered suggested appendicectomy 4% (2/53) surgeons proceeded for diagnostic laparoscopy (Figure 2) to assess whether appendectomy is doable. Regarding interventional radiological drainage, 55% (29/53) surgeons recommended this in the presence of appendicular abscess on CT scan, whereas 17% surgeons (9/53) offered it to the systemically unwell patient only. Approximately two-third of the surgeons (34/53) reported clinical examination and normalization of inflammatory markers as discharge criteria but 26% surgeons (14/53) preferred to perform a repeat CT scan to confirm the complete resolution of appendicular abscess prior to the discharge. Normal practice for follow up investigations was CT scan by 23% (12/53) surgeons, colonoscopy by 13% (7/53) surgeons, combined CT scan and colonoscopy by 57% (30/53) surgeons and approximately 8% (4/53) surgeons did not arrange any investigation after discharging the patients (Figure 3).
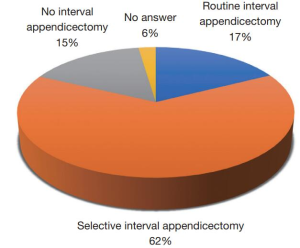
Only 17% (9/53) surgeons offered routine interval appendicectomy and 62% (33/53) offered interval appendicectomy in selective cases of appendicular mass within 6 weeks to 6 months after discharge from the index admission. Eight surgeons (15%) did not offer interval appendicectomy to patients admitted with appendicular mass (Figure 4). When asked about chasing the histopathology report of specimen following operative intervention, 75% (40/53) answered ‘yes’ and around 11% (6/53) answered in selective cases. Rest of the participants answered ‘no’.
Discussion
Brief conclusions
Based upon the findings of this study, the SCAM survey confirms the diverse practice to manage appendicular mass/abscess among surgeons working in South Coast hospitals of England. A substantial percentage of surgeons do not offer interval appendicectomy to patients potentially leaving appendicular and/or caecal neoplastic lesions in situ, the issue raised by a recently published RCT (7).
Strength of current evidence
This study was prompted by the publication of RCT (7) highlighting the need of change of practice towards the recommendation of routine interval appendicectomy in all patients with appendicular mass/abscess following the successful conservative management. This study successfully highlighted the need of change of practice among surgical fraternity in the management of appendicular mass/abscess.
Comparison with previous evidence
To this date, SCAM survey is the first ever study highlighting the diverse practice of the management of appendicular mass in England. Previously published studies have reported same sort of diverse practice highlighting the need of change of practice and reported the risk of appendiceal neoplasia up to 30% in patients undergoing interval appendicectomy (8-11).
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Kim JK, Ryoo S, Oh HK, et al. Management of appendicitis presenting with abscess or mass. J Korean Soc Coloproctol 2010;26:413-9. [Crossref] [PubMed]
- Tannoury J, Abboud B. Treatment options of inflammatory appendiceal masses in adults. World J Gastroenterol 2013;19:3942-50. [Crossref] [PubMed]
- Lane JS, Schmit PJ, Chandler CF, et al. Ileocecectomy is definitive treatment for advanced appendicitis. Am Surg 2001;67:1117-22. [PubMed]
- Brown CV, Abrishami M, Muller M, et al. Appendiceal abscess: immediate operation or percutaneous drainage? Am Surg 2003;69:829-32. [PubMed]
- Varadhan KK, Neal KR, Lobo DN. Safety and efficacy of antibiotics compared with appendicectomy for treatment of uncomplicated acute appendicitis: meta-analysis of randomised controlled trials. BMJ 2012;344:e2156. [Crossref] [PubMed]
- Andersson RE, Petzold MG. Nonsurgical treatment of appendiceal abscess or phlegmon: a systematic review and meta-analysis. Ann Surg. 2007;246:741-8. [Crossref] [PubMed]
- Mällinen J, Rautio T, Grönroos J, et al. Risk of appendiceal neoplasm in periappendicular abscess in patients treated with interval appendectomy vs follow-up with magnetic resonance imaging: 1-year outcomes of the peri-appendicitis acuta randomized clinical trial. JAMA Surg 2019;154:200-7. [Crossref] [PubMed]
- Al-Kurd A, Mizrahi I, Siam B, et al. Outcomes of interval appendectomy in comparison with appendectomy for acute appendicitis. J Surg Res 2018;225:90-4. [Crossref] [PubMed]
- Schwartz JA, Forleiter C, Lee D, et al. Occult appendiceal neoplasms in acute and chronic appendicitis: a single-institution experience of 1793 appendectomies. Am Surg 2017;83:1381-5. [PubMed]
- Enblad M, Birgisson H, Ekbom A, et al. Increased incidence of bowel cancer after non-surgical treatment of appendicitis. Eur J Surg Oncol 2017;43:2067-75. [Crossref] [PubMed]
- Sagebiel TL, Mohamed A, Matamoros A, et al. Utility of appendiceal calcifications detected on computed tomography as a predictor for an underlying appendiceal epithelial neoplasm. Ann Surg Oncol 2017;24:3667-72. [Crossref] [PubMed]
Cite this article as: Sajid MS, Ray K, Hebbar M, Riaz W, Baig MK, Sains P, Singh KK. South Coast appendicular mass management (SCAM) survey. Transl Gastroenterol Hepatol 2020;5:4.