
Enhanced recovery after surgery for gastric cancer (ERAS-GC): optimizing patient outcome
Introduction
In Europe, the end of the 1990s saw the development of a multidisciplinary approach for cancer patients undergoing surgery, particularly in the case of colorectal cancer. The objective was to reduce the surgical stress on the patient and at the same time reduce the cost of hospitalization (1). Different strategies have been proposed under various names, including fast-track surgery, enhanced recovery program, accelerated rehabilitation care, and enforced multimodal rehabilitation care.
Given the growing interest in this field, especially in the West, a specific study group was organized in the context of the European Society of Clinical Nutrition and Metabolism (ESPEN) in 2001. The term enhanced recovery after surgery (ERAS) came into usage for the first time in 2002. Later, in 2009, emerging data from preliminary studies guided the issuance of the first consensus guidelines (2). Soon, principles first adopted in colorectal surgery became more commonly applied in other procedures. However, specific ERAS guidelines for gastric cancer were not published until 2014 (ERAS-GC) (3). Consequently, the literature has little to offer regarding institutions that have adopted an ERAS-GC protocol. In addition, while evidence has been growing in recent years, results are difficult to generalize due to differences in patient characteristics, disease extension, and health systems.
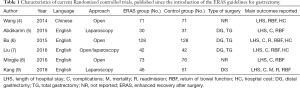
Table 1 summarizes the randomized studies published from the issuing of the ERAS Society guidelines (4-9).
Full table
The ERAS-GC guidelines consist of two sections. The first includes general enhanced recovery items that coincide with the guidelines for pancreaticoduodenectomy (10), while the procedure-specific guidelines contain eight elements (3): preoperative nutrition, preoperative oral pharmaconutrition, access, wound catheters and transversus abdominis plane block, nasogastric/nasojejunal decompression, perianastomotic drains, early postoperative diet and artificial nutrition, and audit. This review offers an analysis of the principles and future perspectives of the ERAS-GC program.
Preoperative nutrition
A recent study, exploring the effects of preoperative nutrition in patients with gastric cancer, showed a direct correlation for both short-term (risk of infection) and long-term survival and disease recovery (11). This finding highlights that adequate nutrition, commencing immediately at the start of the perioperative period, has a considerable impact that cannot be overlooked. In comparison, the guidelines suggest the need to identify patients suffering malnutrition and to determine its severity (3). That said, routine preoperative parenteral nutrition is not recommended in the absence of specific needs.
More recently, randomized trials (12-14) have introduced the concept of immune nutrition, aiming to modulate the systemic inflammatory response. In particular, researchers have found that omega-3 fatty acid and arginine reduce the duration of systemic inflammatory response syndrome and the incidence of infectious postoperative complications (12). Mochiki (13) also described the effect of glutamine on the recovery of intestinal motility. Three reviews and meta-analyses (15-17) related to immunonutrition confirmed that perioperative nutritional support is effective for improving patient immunity and modulating the inflammatory response; however, evidence is lacking concerning the modalities, timing, and characteristics of patients that can receive the most benefit as well as product formulations.
Minimally invasive surgery
The ERAS guidelines (3) recommend the use of minimal-access surgery in order to facilitate short incisions, resulting in less trauma to the tissues. However, in gastric surgery, albeit the use of laparoscopy and robotic surgery is spreading in referral centers, significant debate continues regarding the use of these approaches for advanced gastric cancer (AGC). As another factor in the discussion, AGC represents the majority of patients undergoing surgery in Western countries. Although some authors have published the results of ERAS-GC with open access, minimally invasive surgery represents a fundamental element for the success of an ERAS-based program as it provides support for guaranteeing reduced stress to tissue and rapid physiological recovery.
Authors of systematic reviews and meta-analyses have attempted to define the role of minimally invasive surgery (laparoscopy, robotic surgery, hybrid procedures) for gastric cancer by comparing it with the open approach (18-20). The guidelines describe laparoscopy as a possible alternative to open surgery for early gastric cancer (21); meanwhile, robotic surgery possesses intrinsic technological advantages as articulated instruments may be comfortably controlled from a remote console while offering a 3D view.
Several issues are currently subject to debate in gastric cancer (22,23). Most important is ensuring proper oncological surgery by performing an adequate lymphadenectomy. In randomized trials (19), laparoscopy demonstrated the removal of an adequate number of lymph nodes as required by international guidelines (21).
As another factor, robotic surgery can facilitate better D2 dissection. Advanced technology clearly offers intrinsic advantages for this surgical step, but researchers have not yet proven and verified these through appropriate trials: only four studies (24-27) have contrasted robotic surgery with the open approach, and only one study showed a statistically significant difference in comparison to laparoscopy (28).
Among the intraoperative outcomes, most of the available studies found that minimally invasive surgery led to reduced blood loss. This finding achieved high statistical significance for laparoscopy in Vinuela’s meta-analysis of RCTs (19). Meanwhile, with regard to robotic surgery, a general consensus among different studies has described some advantages over laparoscopy and open surgery in reducing operative bleeding (28,29). Several studies, however, have also reported conflicting results (30,31).
Regarding the post-operative period, the largest RCT (32), performed by the Korean Laparoscopic Gastrointestinal Surgery Study Group, found no significant difference between laparoscopy and open surgery concerning overall complications. In contrast, other studies have shown a significant reduction in medical and minor surgical complications when using laparoscopy (19). Moreover, researchers’ findings have been inconsistent in studies examining robotic surgery when attempting to demonstrate differences compared to laparoscopy in terms of analyzing complications (24,30,33).
Overall, despite the extreme heterogeneity among studies, minimally invasive surgery has demonstrated relevant advantages when compared with open surgery in the area of postoperative hospital stays (20). Some evidence has indicated that patients who underwent robotic gastrectomy could be discharged at an earlier date than patients who underwent open or laparoscopic gastrectomy (34,35). However, the low number of studies in this field along with high heterogeneity weaken this conclusion.
Manually handling organs during surgery is an important contributor to the inflammatory response after surgery (36). Thus, the smaller minimally invasive instruments may cause less inflammation than the instruments used in open surgery.
Nasogastric/nasojejunal decompression
Studies (37,38) concur that the nasogastric/nasojejunal tube should not be used routinely in subjects eligible for the ERAS-GC protocol. The literature has reported no advantage from its routine use (5). In fact, those studies (37,38) have shown that use of the nasogastric tube does not reduce the risk of anastomotic leakage, the number of pulmonary complications, or mortality; in addition, such use significantly reduces the patient’s post-operative comfort. Furthermore, in Yang’s meta-analysis (39), the authors showed that postoperative tube maintenance prolongs postoperative ileus and time to the first flatus. Yamada (40) also reported that complications potentially caused by a shortening of the postoperative fasting period, such as ab-ingestis pneumonia or anastomotic leakage, do not increase under the ERAS protocol.
Perianastomotic drains
The guidelines recommend avoiding the use of abdominal drainage to reduce related complications and accelerate patient recovery (3); however, the level of evidence is low, and only a few cases have been analyzed in a recent meta-analysis of the Cochrane Library (41).
In any event, the absence of abdominal drainage is an additional factor that improves patient comfort as well as stimulates and facilitates walking. While the scientific evidence does not show any benefit in the use of abdominal drainage for numerous surgical procedures (42,43), in the case of gastric surgery, little evidence is available. In particular, the use of drainage after total gastrectomy is still widely debated in the context of the ERAS programs. Therefore, caution is necessary in this case, particularly after extensive lymphadenectomy.
Mobilization
A fundamental item in the ERAS protocol (3) is early mobilization, which is facilitated by the absence of the nasogastric tube and drainage as well as by early removal of the urinary catheter. Smart (44) showed that failure to mobilize patients early is significantly associated with a lengthening of post-operative hospitalization. Many studies (35,40,45,46) have shown that the application of this item of the ERAS program can significantly accelerate the recovery of post-operative intestinal function in comparison to a group subjected to conventional management.
Early postoperative diet
The ERAS protocols require that the patient should not be subjected to long periods of fasting. It has been amply demonstrated that early nutrition reduces postoperative catabolism, accelerates the return of intestinal function, and reduces the risk of complications (47,48). Furthermore, Lewis et al. (49) confirmed in their meta-analysis that keeping patients fasted does not yield any benefit. In fact, although the topic remains controversial, several studies (46,50) have shown that early oral nutrition is not only feasible in gastric surgery but brings significant benefits. Despite the fact that an early dietary recovery has been shown to speed up the patient’s recovery after several surgical procedures, concerns (actually unfounded) related to possible correlation with higher risk of anastomotic leakage or bowel obstruction have caused this approach following gastrectomy to be viewed with distrust. Recent studies (40,51) have confirmed that early feeding after gastrectomy is safe and associated with an improvement in functional recovery and a reduction in hospital stay.
In particular, a randomized controlled trial (52) reported safety data on oral feeding resumption from the second post-operative day after gastrectomy. Studies by Makuuchi (53) and Pedziwiatr (54), comparing the adoption of an ERAS protocol versus conventional management after gastrectomy, confirmed the observation that the recovery of oral nutrition is safe from the second postoperative day. This practice was also found to correlate with a reduction in post-operative administration of intravenous fluids and early discharge (55).
In comparison, Sugisawa (56) focused on evaluating the rate of anastomotic leakage and ab-ingestis pneumonia to assess the real risk attributable to early nutrition. In this study (56), the incidence of anastomotic leakage was 0.8% in the ERAS group, a value not only lower than that of its historical comparison cohort (1.7%) but also in line with or lower than the data rendered by previous studies reporting conventional perioperative management (0.8–1.9%). Therefore, the author concluded that early oral nutrition does not negatively affect the anastomotic site. Yamada (40,57) obtained results that revealed a similar incidence in the rate of leakage (1.1%).
On this topic, the guidelines (3) do not clearly state the different steps to take in resuming oral intake after gastrectomy, but they support an early administration of oral liquids from the first postoperative day. For those patients who are unable to reach at least 60% of the required caloric intake, a tailored nutritional support is recommended. This item, however, is much debated: some authors (58) underline the difficulty in developing specific protocols due to considerable differences regarding type of gastrectomy, stage of disease, and the general condition of the patient.
Perspectives
The effects of adopting an ERAS-GC program depend not only on clinical factors but also on health systems and the socio-cultural substrate of patients. For example, Yamada (40) reported that although ERAS patients had a more rapid functional recovery than those in the conventional group, the length of hospital stay did not differ significantly between the two groups. The authors attributed this result primarily to the Japanese Diagnosis Procedure Combination-based Payment System (DPC) that allows patients to extend their stay at a reduced cost. Among others, Sugisawa (56) reported that the median postoperative hospital stay was significantly reduced in the ERAS group (8 days) compared to its historical cohort (10 days; P=0.001). Wang (46) obtained similar results.
Regarding post-operative complications and the need for reoperations, all studies (35,40,53,56) confirmed the safety of the ERAS approach. Furthermore, they identified no statistically significant difference between the experimental and control groups.
Since the publication of the ERAS-GC guidelines, four meta-analyses (59-62) have been published. Li (61) showed that ERAS-GC with the laparoscopic approach allows a reduction in postoperative hospitalization and reduced costs due to faster recovery without an increase in the readmission rate or complications. In their study, Ding et al. (59) revealed that ERAS improves the postoperative inflammatory response. In addition, Wang (62) reported that ERAS quickens the recovery process with significant reduction in surgical stress and hospitalization costs in addition to improving the nutritional aspects and the quality of life of the patients.
While such evidence is prompting referral centers to adopt strategies, in the spirit of ERAS, to optimize the management of patients with gastric cancer, it is admittedly difficult to generalize the results. In the end, each institution, depending on its needs, should create its own patient-based pathways.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Fearon KC, Ljungqvist O, Von Meyenfeldt M, et al. Enhanced recovery after surgery: a consensus review of clinical care for patients undergoing colonic resection. Clin Nutr 2005;24:466-77. [Crossref] [PubMed]
- Lassen K, Soop M, Nygren J, et al. Consensus review of optimal perioperative care in colorectal surgery: Enhanced Recovery After Surgery (ERAS) Group recommendations. Arch Surg 2009;144:961-9. [Crossref] [PubMed]
- Mortensen K, Nilsson M, Slim K, et al. Consensus guidelines for enhanced recovery after gastrectomy: Enhanced Recovery After Surgery (ERAS(R)) Society recommendations. Br J Surg 2014;101:1209-29. [Crossref] [PubMed]
- Wang G, Yang Y, Zhou B, et al. Promotion of postoperative recovery with fast track surgery for gastric cancer patients undergoing gastrectomy: a prospective randomized controlled study. Zhonghua Wei Chang Wai Ke Za Zhi 2014;17:489-91. [PubMed]
- Abdikarim I, Cao XY, Li SZ, et al. Enhanced recovery after surgery with laparoscopic radical gastrectomy for stomach carcinomas. World J Gastroenterol 2015;21:13339-44. [Crossref] [PubMed]
- Bu J, Li N, Huang X, et al. Feasibility of Fast-Track Surgery in Elderly Patients with Gastric Cancer. J Gastrointest Surg 2015;19:1391-8. [Crossref] [PubMed]
- Liu G, Jian F, Wang X, et al. Fast-track surgery protocol in elderly patients undergoing laparoscopic radical gastrectomy for gastric cancer: a randomized controlled trial. Onco Targets Ther 2016;9:3345-51. [PubMed]
- Mingjie X, Luyao Z, Ze T, et al. Laparoscopic Radical Gastrectomy for Resectable Advanced Gastric Cancer Within Enhanced Recovery Programs: A Prospective Randomized Controlled Trial. J Laparoendosc Adv Surg Tech A 2017;27:959-64. [Crossref] [PubMed]
- Kang SH, Lee Y, Min SH, et al. Multimodal Enhanced Recovery After Surgery (ERAS) Program is the Optimal Perioperative Care in Patients Undergoing Totally Laparoscopic Distal Gastrectomy for Gastric Cancer: A Prospective, Randomized, Clinical Trial. Ann Surg Oncol 2018;25:3231-8. [Crossref] [PubMed]
- Lassen K, Coolsen MM, Slim K, et al. Guidelines for perioperative care for pancreaticoduodenectomy: Enhanced Recovery After Surgery (ERAS(R)) Society recommendations. Clin Nutr 2012;31:817-30. [Crossref] [PubMed]
- Zheng HL, Lu J, Li P, et al. Effects of Preoperative Malnutrition on Short- and Long-Term Outcomes of Patients with Gastric Cancer: Can We Do Better? Ann Surg Oncol 2017;24:3376-85. [Crossref] [PubMed]
- Okamoto Y, Okano K, Izuishi K, et al. Attenuation of the systemic inflammatory response and infectious complications after gastrectomy with preoperative oral arginine and omega-3 fatty acids supplemented immunonutrition. World J Surg 2009;33:1815-21. [Crossref] [PubMed]
- Mochiki E, Ohno T, Yanai M, et al. Effects of glutamine on gastrointestinal motor activity in patients following gastric surgery. World J Surg 2011;35:805-10. [Crossref] [PubMed]
- Fujitani K, Tsujinaka T, Fujita J, et al. Prospective randomized trial of preoperative enteral immunonutrition followed by elective total gastrectomy for gastric cancer. Br J Surg 2012;99:621-9. [Crossref] [PubMed]
- Song GM, Tian X, Liang H, et al. Role of Enteral Immunonutrition in Patients Undergoing Surgery for Gastric Cancer: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Medicine (Baltimore) 2015;94:e1311. [Crossref] [PubMed]
- Song GM, Liu XL, Bian W, et al. Systematic review with network meta-analysis: comparative efficacy of different enteral immunonutrition formulas in patients underwent gastrectomy. Oncotarget 2017;8:23376-88. [PubMed]
- Cheng Y, Zhang J, Zhang L, et al. Enteral immunonutrition versus enteral nutrition for gastric cancer patients undergoing a total gastrectomy: a systematic review and meta-analysis. BMC Gastroenterol 2018;18:11. [Crossref] [PubMed]
- Zong L, Seto Y, Aikou S, et al. Efficacy evaluation of subtotal and total gastrectomies in robotic surgery for gastric cancer compared with that in open and laparoscopic resections: a meta-analysis. PLoS One 2014;9:e103312. [Crossref] [PubMed]
- Viñuela EF, Gonen M, Brennan MF, et al. Laparoscopic versus open distal gastrectomy for gastric cancer: a meta-analysis of randomized controlled trials and high-quality nonrandomized studies. Ann Surg 2012;255:446-56. [Crossref] [PubMed]
- Marano A, Choi YY, Hyung WJ, et al. Robotic versus Laparoscopic versus Open Gastrectomy: A Meta-Analysis. J Gastric Cancer 2013;13:136-48. [Crossref] [PubMed]
- Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer 2017;20:1-19. [Crossref] [PubMed]
- Parisi A, Nguyen NT, Reim D, et al. Current status of minimally invasive surgery for gastric cancer: A literature review to highlight studies limits. Int J Surg 2015;17:34-40. [Crossref] [PubMed]
- Parisi A, Desiderio J. Establishing a multi-institutional registry to compare the outcomes of robotic, laparoscopic, and open surgery for gastric cancer. Surgery 2015;157:830-1. [Crossref] [PubMed]
- Parisi A, Reim D, Borghi F, et al. Minimally invasive surgery for gastric cancer: A comparison between robotic, laparoscopic and open surgery. World J Gastroenterol 2017;23:2376-84. [Crossref] [PubMed]
- Kim MC, Heo GU, Jung GJ. Robotic gastrectomy for gastric cancer: surgical techniques and clinical merits. Surg Endosc 2010;24:610-5. [Crossref] [PubMed]
- Kim KM, An JY, Kim HI, et al. Major early complications following open, laparoscopic and robotic gastrectomy. Br J Surg 2012;99:1681-7. [Crossref] [PubMed]
- Huang KH, Lan YT, Fang WL, et al. Initial experience of robotic gastrectomy and comparison with open and laparoscopic gastrectomy for gastric cancer. J Gastrointest Surg 2012;16:1303-10. [Crossref] [PubMed]
- Junfeng Z, Yan S, Bo T, et al. Robotic gastrectomy versus laparoscopic gastrectomy for gastric cancer: comparison of surgical performance and short-term outcomes. Surg Endosc 2014;28:1779-87. [Crossref] [PubMed]
- Kang BH, Xuan Y, Hur H, et al. Comparison of Surgical Outcomes between Robotic and Laparoscopic Gastrectomy for Gastric Cancer: The Learning Curve of Robotic Surgery. J Gastric Cancer 2012;12:156-63. [Crossref] [PubMed]
- Son T, Lee JH, Kim YM, et al. Robotic spleen-preserving total gastrectomy for gastric cancer: comparison with conventional laparoscopic procedure. Surg Endosc 2014;28:2606-15. [Crossref] [PubMed]
- Eom BW, Yoon HM, Ryu KW, et al. Comparison of surgical performance and short-term clinical outcomes between laparoscopic and robotic surgery in distal gastric cancer. Eur J Surg Oncol 2012;38:57-63. [Crossref] [PubMed]
- Kim HH, Hyung WJ, Cho GS, et al. Morbidity and mortality of laparoscopic gastrectomy versus open gastrectomy for gastric cancer: an interim report--a phase III multicenter, prospective, randomized Trial (KLASS Trial). Ann Surg 2010;251:417-20. [Crossref] [PubMed]
- Hyun MH, Lee CH, Kwon YJ, et al. Robot versus laparoscopic gastrectomy for cancer by an experienced surgeon: comparisons of surgery, complications, and surgical stress. Ann Surg Oncol 2013;20:1258-65. [Crossref] [PubMed]
- Woo Y, Hyung WJ, Pak KH, et al. Robotic gastrectomy as an oncologically sound alternative to laparoscopic resections for the treatment of early-stage gastric cancers. Arch Surg 2011;146:1086-92. [Crossref] [PubMed]
- Desiderio J, Stewart CL, Sun V, et al. Enhanced Recovery after Surgery for Gastric Cancer Patients Improves Clinical Outcomes at a US Cancer Center. J Gastric Cancer 2018;18:230-41. [Crossref] [PubMed]
- Hiki N, Shimizu N, Yamaguchi H, et al. Manipulation of the small intestine as a cause of the increased inflammatory response after open compared with laparoscopic surgery. Br J Surg 2006;93:195-204. [Crossref] [PubMed]
- Carrère N, Seulin P, Julio CH, et al. Is nasogastric or nasojejunal decompression necessary after gastrectomy? A prospective randomized trial. World J Surg 2007;31:122-7. [Crossref] [PubMed]
- Suehiro T, Matsumata T, Shikada Y, et al. Accelerated rehabilitation with early postoperative oral feeding following gastrectomy. Hepatogastroenterology 2004;51:1852-5. [PubMed]
- Yang Z, Zheng Q, Wang Z. Meta-analysis of the need for nasogastric or nasojejunal decompression after gastrectomy for gastric cancer. Br J Surg 2008;95:809-16. [Crossref] [PubMed]
- Yamada T, Hayashi T, Cho H, et al. Usefulness of enhanced recovery after surgery protocol as compared with conventional perioperative care in gastric surgery. Gastric Cancer 2012;15:34-41. [Crossref] [PubMed]
- Wang Z, Chen J, Su K, et al. Abdominal drainage versus no drainage post-gastrectomy for gastric cancer. Cochrane Database Syst Rev 2015.CD008788. [PubMed]
- Kawai M, Tani M, Terasawa H, et al. Early removal of prophylactic drains reduces the risk of intra-abdominal infections in patients with pancreatic head resection: prospective study for 104 consecutive patients. Ann Surg 2006;244:1-7. [Crossref] [PubMed]
- Petrowsky H, Demartines N, Rousson V, et al. Evidence-based value of prophylactic drainage in gastrointestinal surgery: a systematic review and meta-analyses. Ann Surg 2004;240:1074-84; discussion 1084-5. [Crossref] [PubMed]
- Smart NJ, White P, Allison AS, et al. Deviation and failure of enhanced recovery after surgery following laparoscopic colorectal surgery: early prediction model. Colorectal Dis 2012;14:e727-34. [Crossref] [PubMed]
- Teeuwen PH, Bleichrodt RP, Strik C, et al. Enhanced recovery after surgery (ERAS) versus conventional postoperative care in colorectal surgery. J Gastrointest Surg 2010;14:88-95. [Crossref] [PubMed]
- Wang D, Kong Y, Zhong B, et al. Fast-track surgery improves postoperative recovery in patients with gastric cancer: a randomized comparison with conventional postoperative care. J Gastrointest Surg 2010;14:620-7. [Crossref] [PubMed]
- Han-Geurts IJ, Hop WC, Kok NF, et al. Randomized clinical trial of the impact of early enteral feeding on postoperative ileus and recovery. Br J Surg 2007;94:555-61. [Crossref] [PubMed]
- Lewis SJ, Egger M, Sylvester PA, et al. Early enteral feeding versus "nil by mouth" after gastrointestinal surgery: systematic review and meta-analysis of controlled trials. BMJ 2001;323:773-6. [Crossref] [PubMed]
- Lewis SJ, Andersen HK, Thomas S. Early enteral nutrition within 24 h of intestinal surgery versus later commencement of feeding: a systematic review and meta-analysis. J Gastrointest Surg 2009;13:569-75. [Crossref] [PubMed]
- Jo DH, Jeong O, Sun JW, et al. Feasibility study of early oral intake after gastrectomy for gastric carcinoma. J Gastric Cancer 2011;11:101-8. [Crossref] [PubMed]
- Scatizzi M, Kroning KC, Boddi V, et al. Fast-track surgery after laparoscopic colorectal surgery: is it feasible in a general surgery unit? Surgery 2010;147:219-26. [Crossref] [PubMed]
- Hur H, Kim SG, Shim JH, et al. Effect of early oral feeding after gastric cancer surgery: a result of randomized clinical trial. Surgery 2011;149:561-8. [Crossref] [PubMed]
- Makuuchi R, Sugisawa N, Kaji S, et al. Enhanced recovery after surgery for gastric cancer and an assessment of preoperative carbohydrate loading. Eur J Surg Oncol 2017;43:210-7. [Crossref] [PubMed]
- Pędziwiatr M, Matlok M, Kisialeuski M, et al. Short hospital stays after laparoscopic gastric surgery under an Enhanced Recovery After Surgery (ERAS) pathway: experience at a single center. Eur Surg 2014;46:128-32. [Crossref] [PubMed]
- Terashima M. The earlier the better? Gastric Cancer 2014;17:197-9. [Crossref] [PubMed]
- Sugisawa N, Tokunaga M, Makuuchi R, et al. A phase II study of an enhanced recovery after surgery protocol in gastric cancer surgery. Gastric Cancer 2016;19:961-7. [Crossref] [PubMed]
- Yamada T, Hayashi T, Aoyama T, et al. Feasibility of enhanced recovery after surgery in gastric surgery: a retrospective study. BMC Surg 2014;14:41. [Crossref] [PubMed]
- Shimizu N, Oki E, Tanizawa Y, et al. Effect of early oral feeding on length of hospital stay following gastrectomy for gastric cancer: a Japanese multicenter, randomized controlled trial. Surg Today 2018;48:865-74. [Crossref] [PubMed]
- Ding J, Sun B, Song P, et al. The application of enhanced recovery after surgery (ERAS)/fast-track surgery in gastrectomy for gastric cancer: a systematic review and meta-analysis. Oncotarget 2017;8:75699-711. [PubMed]
- Li Z, Wang Q, Li B, et al. Influence of enhanced recovery after surgery programs on laparoscopy-assisted gastrectomy for gastric cancer: a systematic review and meta-analysis of randomized control trials. World J Surg Oncol 2017;15:207. [Crossref] [PubMed]
- Li MZ, Wu WH, Li L, et al. Is ERAS effective and safe in laparoscopic gastrectomy for gastric carcinoma? A meta-analysis. World J Surg Oncol 2018;16:17. [Crossref] [PubMed]
- Wang LH, Zhu RF, Gao C, et al. Application of enhanced recovery after gastric cancer surgery: An updated meta-analysis. World J Gastroenterol 2018;24:1562-78. [Crossref] [PubMed]
Cite this article as: Desiderio J, Trastulli S, D’Andrea V, Parisi A. Enhanced recovery after surgery for gastric cancer (ERAS-GC): optimizing patient outcome. Transl Gastroenterol Hepatol 2020;5:11.


