Palliative chemotherapy in pancreatic cancer—treatment sequences
First line options for palliative chemotherapy in pancreatic cancer
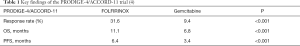
For years, gemcitabine has been the standard of care and the only therapeutic option in patients with metastatic pancreatic cancer (mPC). The benefit of gemcitabine treated patients in stage IV pancreatic cancer was very limited with 5.65 months (1). Subsequent phase II and phase III studies that aimed to improve the outcome of gemcitabine in combination with different compounds over gemcitabine monotherapy failed. The first positive trial was published in 2007. In this study gemcitabine with erlotinib, a potent and selective epidermal growth factor receptor (EGFR) tyrosine kinase inhibitor, revealed a statistically, albeit clinically not really meaningful benefit of 0.33 months (2). However, patients that developed a skin rash showed a hitherto unknown extension of overall survival with up to 11 months (3). This association has been confirmed in subsequent studies. In 2011 and 2013 data of two phase III studies were released showing a statistically relevant and clinically meaningful improvement in the overall survival of mPC patients thus providing two first line chemotherapeutic options. The PRODIGE-4/ACCORD-11 trial investigated the benefits of therapy with FOLFIRINOX compared with gemcitabine. In this study the treatment with FOLFIRINOX showed an objective response rate of approximately 31.6% and a median overall survival of 11.1 versus 6.8 months in the gemcitabine mono cohort (4) (Table 1). These data were very encouraging demonstrating for the first time not only a nearly doubling of the overall survival, but also high objective response rates. And yet, it has to be noted that in this PRODIGE trial a highly selective patient cohort was chosen with patients included who were under an age of 76 years with an ECOG of 0 or 1, sufficient renal and liver function (bilirubin up to <1.5 of the norm), a bone marrow with a granulocyte count of ≥1,500 mm2 as well as a plated count of ≥100,000 mm2. In a less highly selective patient cohort the MPACT trial investigated the effects of a chemotherapy with gemcitabine/nab-paclitaxel compared with gemcitabine alone. The objective response rate for gemcitabine/nab-paclitaxel was 23% and the median overall survival 8.5 months (5) (Table 2). The MPACT trial included older patients in slightly reduced general condition with a Karnofsky index of up to 70 with an adequate bone marrow (neutrophile count ≥1.5×109/L, hemoglobin ≥9 g/dL) and adequate renal function as well as a bilirubin level below the upper limit of the normal range. As expected, due to the potent combination of drugs in these regimens, more toxicities like hematotoxicity and polyneuropathy were registered. In general, the FOLFIRINOX regimen showed a higher side effect rate than gemcitabine/nab-paclitaxel with the exception of polyneuropathy which occurred more frequently in the treatment with gemcitabine/ nab-paclitaxel.
FOLFIRINOX or gemcitabine/nab-paclitaxel: which to choose?
The choice of any first line chemotherapy depends on the general condition and comorbidities of the patient. According to the PRODIGE-4/ACCORD-11 study a patient in an excellent general condition under the age of 76 without severe comorbidities would most likely be treated with the FOLFIRINOX regimen whereas according to the MPACT trial the treatment with gemcitabine/nab-paclitaxel would be preferred in an older patient in a slightly reduced general condition. Interestingly, those patients with high tumor marker CA 19-9 and high tumor load seem to benefit from gemcitabine/nab-paclitaxel even more. In this subgroup the greatest reduction in the risk of death as well as a greater progression free survival was noted. For both regimens normal or slightly elevated bilirubin is a prerequisite. Therefore, high levels of bilirubin due to cholestasis have to be normalized through endoscopic drainage of biliary stenosis. Due to the high toxicity of FOLFIRINOX patients are frequently treated with a dose reduced modified FOLFIRINOX protocol instead of the original FOLFIRINOX regimen. In 2016 a phase II trial investigated the effects of modified FOLFIRINOX as a first line therapy in locally advanced and mPCs (6). In locally advanced tumors the use of modified FOLFIRINOX led to a response rate of 17.2%, a resection rate of 41.9% and an overall survival of 26.6 months. In metastatic disease the response rate was 35.1% and the overall survival 10.2 months. As expected, the use of modified FOLFIRINOX led to a lower rate of adverse events. Thus, modified FOLFIRINOX might prove itself an effective but less toxic alternative to the original FOLFIRINOX protocol.
Having observed the high toxicities with both regimens recent efforts were undertaken to establish maintenance therapies. Recently, preliminary data from the PRODIGE 35-PANOPTIMOX trial showed that a maintenance therapy with 5-FU after 8 cycles of FOLFIRINOX is a safe strategy (7). A treatment with FOLFIRINOX should especially be considered in patients with a family history for BRCA associated cancers like breast, prostate and pancreatic cancer. BRCA1 or BRCA2 mutations increase sensitivity of pancreatic cancers towards platin-based therapies due to the lack of an efficient DNA repair system (8), Such patients were shown to display high sensitivities towards FOLFIRINOX. The POLO trial (olaparib as maintenance treatment following first-line platinum-based chemotherapy in patients with a germline BRCA mutation and metastatic pancreatic cancer) has investigated the efficacy of olaparib, a PARP-inhibitor, as a maintenance therapy in germline BRCA-mutated pancreatic cancer who did not progress under platinum-based first line therapy (e.g., FOLFIRINOX). Data from this trial indeed suggest a significant prolongation of progression-free survival under the maintenance therapy with olaparib (9). Likewise, current efforts to establish modifications of gemcitabine/nab-paclitaxe are under way and urgently needed as neuropathy as the main side effect affects the quality of life.
For all patients who are not eligible for both regimens either due to the general conditions, or preexisting comorbidities (such as diabetic PNP) gemcitabine with or without erlotinib is still an option. In the absence of skin rash after 4–6 weeks of therapy erlotinib has to be terminated. The absence of skin rash under erlotinib therapy is a predictive marker for the efficacy of erlotinib. In patients with high bilirubin due to untreatable cholestasis or impaired liver function, best supportive care has to be considered.
Recent developments in Asian cohorts have shed new light on S1, an oral 5-FU prodrug. The GEST-trail investigated the effects of S1 compared to gemcitabine in locally advanced and mPC. In this study S1 showed to be at least equally effective as gemcitabine whilst less toxic (10). The NPSPAC trial investigated the effects of a therapy with S1/nab-paclitaxel compared to gemcitabine in advanced pancreatic cancer. The combination of S1/nab-paclitaxel showed an objective response rate of approximately 50% and an overall survival of 9.4 months. The subgroup analysis showed a significant benefit in progression free survival (7.7 vs. 5.0 months) as well as in overall survival (18.2 vs. 8.5 months) of the female subgroup compared to the male subgroup (11). Regarding the tolerability of S1 this combination might therefore become an alternative regimen. However, this data is yet restricted to Asian patients. The relevance of S1 in western populations in general and in pancreatic cancer in particular is unclear as metabolism of the prodrug seems to differ between Asian and western population.
Second line options for palliative chemotherapy in pancreatic cancer
Despite the dismal prognosis, the aggressive chemotherapeutic regimens and their side effects around 50% of patients with mPC will require a second-line chemotherapy. Recently, for these patients second-line chemotherapies have been established. The choice of the second line treatment depends on the compounds used as first line therapy, the side-effects/toxicities and the general patient´s condition.
Second line options after first line treatment with FOLFIRINOX
After the use of FOLFIRINOX gemcitabine-based regimens should be considered as primary options. If the patient is still in an acceptable general condition and doesn’t suffer from polyneuropathy gemcitabine/nap-paclitaxel might be a feasible option. A prospective phase II study showed an objective response rate of 17.5% and a median overall survival of 8.8 months for the use of gemcitabine/nap-paclitaxel after FOLFIRINOX (12). If the patient is already in a reduced general condition gemcitabine/erlotinib or gemcitabine mono represent options which should be considered. In retrospective studies, the use of gemcitabine as second line treatment led to a median overall survival from 3.6 up to 5.7 months (13,14).
Second line options after first line treatment with gemcitabine-based regimens
After failure of a gemcitabine-based chemotherapy 5-FU-based regimens are valid options. As part of the CONKO-003 trial the effects of the OFF regimen in a second line setting in gemcitabine refractory pancreatic cancers were investigated. The use of the OFF regimen led to an improved overall survival of 5.9 months compared to 3.3 months in the control arm (5-FU/folinic acid) (15,16). However, after a first line treatment with gemcitabine/nab-paclitaxel the use of the OFF regimen might be prevented by preexisting polyneuropathy. Another option was presented by the NAOPOLI-1 trial. This study investigated the effects of a combination of lip. irinotecan, 5-FU and folinic acid after failure of a gemcitabine-based chemotherapy. The trial showed a median overall survival of 6.1 months in the lip-irinotecan group compared to 4.2 months in the 5-FU/folinic acid group (17) (Table 3). A less frequent used option is the FOLFIRI regimen which may achieve an overall survival of approximately 5 months in the second line setting (18). Selected patients who are still in a very good general condition after gemcitabine-based first line therapy and don’t suffer from polyneuropathy might be considered for the FOLFIRINOX regimen though there are no data for the use of FOLFIRINOX in a second-line setting. The effects of the FOLFOX regimen in a second line setting after a gemcitabine-based therapy was investigated in the PANCREOX trial. Unfortunately, besides increased toxicity, the use of FOLFOX resulted in a worse overall survival of 6.1 months compared to 9.9 months in the 5-FU/leucovorin control (19).
An explanation for the worse outcome under the application of FOLFOX compared to the benefit of the OFF regimen in the CONKO-003 trial might be the different amount of oxaliplatin. In both regimen oxaliplatin is administered with a dose of 85 mg/m2. Though in the OFF regimen oxaliplatin is administered on day 8 and 22 of a q42 cycle, while the FOLFOX regimen use oxaliplatin in a q14 cycle, which means the cumulative dose of oxaliplatin is much higher in the FOLFOX regimen. Based on the current data FOLFOX shouldn’t be recommended outside of clinical trials.
Third line options for palliative chemotherapy in pancreatic cancer
After undergoing two lines of systemic chemotherapy only a minority of approximately 25–30% of the patients is still in the condition for further treatment. The only phase III trial which included third line treatment is the NAPOLI-1 trial. In this study approximately 30% of the included patients had already received at least 2 lines of chemotherapy. Therefore, the combination of 5-FU/leucovorin/lip-irinotecan is the only validated third line option after previous gemcitabine-based therapy. At present, there are no data for a third line option after previous 5-FU-based regimens.
New approaches and individualized treatment in pancreatic cancer
Thanks to the new possibilities in genetic analysis we now can sequence tumor tissues in order to find druggable mutations as individualized targets. Unfortunately, even if mutations are found in most of the cases specific compounds targeting these structures are lacking. However, some approaches seem quite promising. As previously mentioned, a maintenance therapy with PARP inhibitors might become a new approach in cancers with a germline BRCA1 or BRCA2 mutation. Other interesting mutations are fusions of the receptor tyrosine kinases NTRK and ROS1. Pishvaian et al. used the selective TRK and ROS1 inhibitor entrectinib in patients with the appropriate mutations in a small phase II trial. The use of the drug led to a partial response with normalization of CA 19-9 marker and only minor side effects were noted (20). Another important genetic factor is the activation of the RAS pathway. Although mutations in the RAS pathway are already known as major players in the development of a greater part of the pancreatic cancers, until recently, a compound directly inhibiting the effect of mutated KRAS has not reached the clinic yet; thus, this target has been considered as non-druggable. However, currently many efforts are underway to target mutated KRAS through combination therapies, as previously described with trametinib and autophagy blocker chloroquine or MEK-inhibitors with the allosteric SHP2-inhibitors (21,22). The use of trametinib together with chloroquine for example led to a decrease of the CA 19-9 levels by 95% as well as to a decrease of the tumor burden in the CT scan by 50% (23). Further investigation is needed to confirm the success of this combination but in suitable patients with no other alternatives of treatment it might represent another option. While in most cases a genetic analysis is used as a last approach to find a suitable therapy there are interesting new developments which might help to decide which therapy should be administered to a patient. Tiriac et al. recently identified signatures which could be used to predict the response to a therapy by using organoid profiling (24). So maybe, we will be able to choose the therapy not only by considering factors like general condition and age but also by the genetic profile of a cancer.
Conclusion and sequence therapy in pancreatic cancer
Depending on the general condition, comorbidities and age of the patient a first line therapy with FOLFIRINOX or gemcitabine/nab-paclitaxel should be considered in patients as primary options. Gemcitabine in combination with erlotinib or as monotherapy are still options for patients in a reduced condition. After the failure of FOLFIRINOX, a gemcitabine-based therapy especially gemcitabine/nab-paclitaxel but also gemcitabine/erlotinib or gemcitabine alone should be considered as second line options. After the failure of a gemcitabine based first line therapy, 5-FU-based regimens such as OFF or lip-irinotecan/5-FU/folinic acid have to be considered. In addition, lip-irinotecan/5-FU/folinic acid may be used as third line option. A recent study (JAMA) has suggested that genetic mutations that can be inherited (germline mutations) are more prevalent than previously thought. Thus, genetic tests in patients with pancreatic cancer should be encouraged, regardless of family history (25).
Acknowledgments
None.
Footnote
Conflicts of Interest: H Algül: receives honoraria from Servier and Celgene and research funding from Chugai. R Abbassi has no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Burris HA 3rd, Moore MJ, Andersen J, et al. Improvements in survival and clinical benefit with gemcitabine as first-line therapy for patients with advanced pancreas cancer: a randomized trial. J Clin Oncol 1997;15:2403-13. [Crossref] [PubMed]
- Moore MJ, Goldstein D, Hamm J, et al. Erlotinib plus gemcitabine compared with gemcitabine alone in patients with advanced pancreatic cancer: a phase III trial of the National Cancer Institute of Canada Clinical Trials Group. J Clin Oncol 2007;25:1960-6. [Crossref] [PubMed]
- Aranda E., Manzano JL, Rivera F, et al. Phase II open-label study of erlotinib in combination with gemcitabine in unresectable and/or metastatic adenocarcinoma of the pancreas: relationship between skin rash and survival (Pantar study). Ann Oncol 2012;23:1919-25. [Crossref] [PubMed]
- Conroy T, Desseigne F, Ychou M, et al. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med 2011;364:1817-25. [Crossref] [PubMed]
- Von Hoff DD, Ervin T, Arena FP, et al. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N Engl J Med 2013;369:1691-703. [Crossref] [PubMed]
- Stein SM, James ES, Deng Y, et al. Final analysis of a phase II study of modified FOLFIRINOX in locally advanced and metastatic pancreatic cancer. Br J Cancer 2016;114:737-43. [Crossref] [PubMed]
- Laetitia D, Jean MP, Le Malicot K, et al. FOLFIRINOX until progression, FOLFIRINOX with maintenance treatment, or sequential treatment with gemcitabine and FOLFIRI.3 for first-line treatment of metastatic pancreatic cancer: A randomized phase II trial (PRODIGE 35-PANOPTIMOX). J Clin Oncol 2018;36:4000. [Crossref]
- Aung KL, Holter S, Borgida A, et al. Overall survival of patients with pancreatic adenocarcinoma and BRCA1 or BRCA2 germline mutation. J Clin Oncol 2016;34:4123. [Crossref]
- Golan T, Hammel P, Reni M, et al. Maintenance Olaparib for Germline BRCA-Mutated Metastatic Pancreatic Cancer. N Engl J Med 2019. [Epub ahead of print]. [Crossref] [PubMed]
- Ueno H, Ikeda M, Ohkawa S, et al. Randomized phase III study of gemcitabine plus S-1, S-1 alone, or gemcitabine alone in patients with locally advanced and metastatic pancreatic cancer in Japan and Taiwan: GEST study. J Clin Oncol 2013;31:1640-8. [Crossref] [PubMed]
- Shi Y, Zhang S, Han Q, et al. Nab-paclitaxel plus S-1 in advanced pancreatic adenocarcinoma (NPSPAC): a single arm, single center, phase II trial. Oncotarget 2017;8:92401-10. [Crossref] [PubMed]
- Portal A, Pernot S, Tougeron D, et al. Nab- paclitaxel plus gemcitabine for metastatic pancreatic adenocarcinoma after FOLFIRINOX failure: an AGEO prospective multicentre cohort. Br J Cancer 2015;113:989-95. [Crossref] [PubMed]
- Sarabi M, Mais L, Oussaid N, et al. Use of gemcitabine as a second-line treatment following chemotherapy with folfirinox for metastatic pancreatic adenocarcinoma. Oncol Lett 2017;13:4917-24. [Crossref] [PubMed]
- da Rocha Lino A, Abrahão CM, Brandão RM, et al. Role of gemcitabine as second-line therapy after progression on FOLFIRINOX in advanced pancreatic cancer: a retrospective analysis. J Gastrointest Oncol 2015;6:511-5. [PubMed]
- Pelzer U, Schwaner I, Stieler J, et al. Best supportive care (BSC) versus oxaliplatin, folinic acid and 5-fluorouracil (OFF) plus BSC in patients for second-line advanced pancreatic cancer: a phase III-study from the German CONKO-study group. Eur J Cancer 2011;47:1676-81. [Crossref] [PubMed]
- Oettle H, Riess H, Stieler JM, et al. Second-line oxaliplatin, folinic acid, and fluorouracil versus folinic acid and fluorouracil alone for gemcitabine-refractory pancreatic cancer: outcomes from the CONKO-003 trial. J Clin Oncol 2014;32:2423-9. [Crossref] [PubMed]
- Wang-Gillam A, Li CP, Bodoky G, et al. Nanoliposomal irinotecan with fluorouracil and folinic acid in metastatic pancreatic cancer after previous gemcitabine-based therapy (NAPOLI-1): a global, randomised, open-label, phase 3 trial. Lancet 2016;387:545-57. [Crossref] [PubMed]
- Zaniboni A, Aitini E, Barni S, et al. FOLFIRI as second-line chemotherapy for advanced pancreatic cancer: a GISCAD multicenter phase II study. Cancer Chemother Pharmacol 2012;69:1641-5. [Crossref] [PubMed]
- Gill S, Ko YJ, Cripps C, et al. PANCREOX: A randomized phase III study of fluorouracil/leucovorin with or without oxaliplatin for second-line advanced pancreatic cancer in patients who have received gemcitabine-based chemotherapy. J Clin Oncol 2016;34:3914-20. [Crossref] [PubMed]
- Pishvaian MJ, Rolfo CD, Liu SV, et al. Clinical benefit of entrectinib for patients with metastatic pancreatic cancer who harbor NTRK and ROS1 fusions. J Clin Oncol 2018;36:521. [Crossref]
- Pishvaian MJ, Garrido-Laguna I, Liu SV, et al. Entrectinib in TRK and ROS1 fusion-positive metastatic pancreatic cancer. JCO Precision Oncology 2018;2:1-7. [Crossref]
- Ruess DA, Heynen GJ, Ciecielski KJ, et al. Mutant KRAS-driven cancers depend on PTPN11/SHP2 phosphatase. Nat Med 2018;24:954-60. [Crossref] [PubMed]
- Kinsey CG, Camolotto SA, Boespflug AM, et al. Protective autophagy elicited by RAF→MEK→ERK inhibition suggests a treatment strategy for RAS-driven cancers. Nat Med 2019;25:620-7. [Crossref] [PubMed]
- Tiriac H, Belleau P, Engle DD, et al. Organoid profiling identifies common responders to chemotherapy in pancreatic cancer. Cancer Discov 2018;8:1112-9. [Crossref] [PubMed]
- Hu C, Hart SN, Polley EC, et al. Association Between Inherited Germline Mutations in Cancer Predisposition Genes and Risk of Pancreatic Cancer. JAMA 2018;319:2401-9. [Crossref] [PubMed]
Cite this article as: Abbassi R, Algül H. Palliative chemotherapy in pancreatic cancer—treatment sequences. Transl Gastroenterol Hepatol 2019;4:56.