
Treatment of pancreatic cancer—neoadjuvant treatment in resectable pancreatic cancer (PDAC)
Pancreatic cancer—even if deemed resectable—has still a dismal prognosis. Surgical treatment of pancreatic ductal adenocarcinoma (PDAC) has substantially improved over the last years and perioperative morbidity and mortality is at an all-time low particularly in high volume centers. It appears therefore unlikely that further improvements in surgical treatment will substantially improve the outcome of patients with PDAC. Multimodal therapies, in particular neoadjuvant chemotherapy and radiochemotherapy, have substantially improved the outcome of other resectable gastrointestinal (GI) cancers such as esophagus and gastric cancer. It is reasonable to assume that efficient chemotherapy and or radiochemotherapy may have a similar impact on the outcome of resectable PDAC. It is important to note that the focus of this paper is on a truly neoadjuvant approach, i.e., neoadjuvant and perioperative treatment of resectable PDAC. We will not consider downsizing strategies to improve R0 resectability in borderline resectable PDAC or induction treatments to enable resectability of locally advanced PDAC.
Adjuvant treatment—the standard of care
Neoadjuvant treatment of PDAC is at present still experimental. The current standard of care is upfront resection and adjuvant chemotherapy either with Gemcitabine or with a combination chemotherapy. Recently, a modified FOLFIRINOX (mFOLFIRINOX) protocol has demonstrated tremendous efficacy in the adjuvant setting compared to Gemcitabine alone with a median disease-free survival (mDFS) of 21.6 months compared to 12.8 months and a 3-year DFS rate of 39.7% compared to 21.4% with Gemcitabine alone. The mFOLFIRINOX protocol was superior to Gemcitabine in virtually all subgroups analyzed including patients with T3/4 tumors, N+ tumors, R1 resection and poorly or undifferentiated tumors. The inclusion criteria for the trial were rather strict (ECOG 0-1, no R2 resections, no CA 19-9 >180 U/mL post-surgery, no uncontrolled diarrhea post-surgery and no bowel obstruction). The median age of 63 years in the trial suggests that the majority of patients included were younger than the average population of patients with PDAC (1). It is also important to note that only about 60% of the patients with PDAC receive adjuvant treatment in the real world due to perioperative morbidity even if one extends the start of adjuvant treatment up to 3 months postoperatively (2).
Neoadjuvant treatment—the pros and cons
There are several arguments in favour of neoadjuvant treatment. First of all, efficient downsizing of the tumor could result in a substantial increase in the proportion of R0 resections which we know is prognostic (3,4). There are also data suggesting that neoadjuvant chemotherapy may be more efficient than adjuvant treatment due to a preserved anatomy and vasculature and due to a higher dose intensity in the neoadjuvant setting (5). There is also the systemic effect of neoadjuvant chemotherapy that has to be considered. There are data suggesting that the majority of PDACs is likely to exhibit micrometastases even when only a small primary tumor is detectable by clinical imaging leading to early relapse and death after surgery in the majority of cases (6). Efficient chemotherapy could treat these micrometastases and prevent early relapse post-surgery. From a patient’s point of view, it can be considered that neoadjuvant treatment for a defined short period is in general better tolerated than the same treatment after extensive surgery. Neoadjuvant treatment also provides a “window of opportunity” to get to know the biology of a respective tumor. There will be tumors (about 20%) progressing during neoadjuvant treatment and even become unresectable (3,4). However, it is fair to say that it is unlikely that a patient with a tumor progressing rapidly under efficient chemotherapy in a short timeframe of 2–3 months would have been cured by upfront surgery, in particular since in many cases progress is not due to progress of the primary tumor, but due to the occurrence of distant metastases, e.g., in the liver. Nevertheless, this topic needs to be addressed in randomized trials.
According to the current guidelines, surgery of PDAC can be performed without prior histological confirmation (7). However, when neoadjuvant treatment is planned a definitive histological or at least cytological diagnosis of PDAC is required before starting chemotherapy. Alas in up to 25% of cases there is not sufficient material obtainable even by repeated EUS-guided FNA to obtain such a diagnosis and surgery gets delayed without neoadjuvant treatment being started (8). Alternative means such as analyzing mutant KRAS [detectable in about 95% of PDACs (tissue based)] in liquid biopsies have so far not shown sufficient sensitivity and specificity in patients with resectable PDAC to substitute tissue analysis. The KRAS mutation rate in plasma/serum was only about 31% compared to 82% in the tumor tissue (9). A way forward may be the use of composite liquid markers. Recently we could show that a combination of circulating free DNA quantification, thrombospondin and CA 19-9 exhibits a c-statistics of 0.9 even for stage I PDAC compared to 0.69 for CA 19-9 alone (10).
Finally, neoadjuvant treatment may improve the outcome, but this has to be weighed against the toxicity of the treatment affecting potentially perioperative morbidity and even mortality. This is particularly important when more aggressive chemotherapy protocols are used.
Neoadjuvant treatment—the data
As stated above neoadjuvant treatment of resectable PDAC is still experimental and there are as yet few data from prospective, randomized, controlled trials. Due to a rather generous use of the term “neoadjuvant treatment” for resectable, but also for borderline resectable and locally advanced tumors in the literature it is sometimes difficult to extract data exclusively for the resectable situation.
Older systematic reviews and meta-analyses found an only marginal efficacy of a neoadjuvant treatment for resectable tumors. Using the chemotherapy protocols available at that time resection rates and survival data of neoadjuvant treatment were comparable with those from upfront surgery plus adjuvant treatment (3,4,11).
However, we know that the efficacy of the neoadjuvant treatment—as determined by pathological tumor response—is paramount for improving survival (12). With the more recent combination chemotherapy protocols such as FOLFIRINOX and Gemcitabine plus nab-Paclitaxel we have more efficient tools in our hands.
A systematic review employed a Markov decision analysis to compare the life expectancy and quality-adjusted life expectancy of neoadjuvant treatment or upfront surgery in resectable PDAC. The authors searched the literature between 2000 and 2015. Twenty-two out of 786 studies fulfilled the criteria. Neoadjuvant treatment resulted in a higher life expectancy (32.2 vs. 26.7 months) as well as a higher quality adjusted life expectancy (25.5 vs. 20.8 months) (13).
A more recent propensity scores matched analysis included 14,941 patients in the analysis. A 3:1 matching by propensity was performed and finally 6,016 patients with upfront resection and 2005 patients with neoadjuvant treatment plus resection were examined. The authors state that neoadjuvant treatment has a significant beneficial effect on T stage, lymph nodes and resection margins. Neoadjuvant treatment improved overall survival (OS) compared to both, upfront surgery alone (HR =0.73; 95% CI: 0.68–0.76) or surgery plus adjuvant treatment (HR =0.83; 95% CI: 0.78–0.89). Neoadjuvant treatment was an independent predictor of lower mortality in the matched data set with an adjusted HR of 0.74 compared to upfront resection (95% CI: 0.69–0.79) (14).
Apart from these retrospective evaluations the first prospective trials examining neoadjuvant treatment in resectable PDAC are available. A Dutch trial compared upfront surgery plus adjuvant Gemcitabine treatment for 6 cycles with neoadjuvant radiochemotherapy consisting of preoperative Gemcitabine treatment and Gemcitabine-based radiochemotherapy as well as 4 cycles of postoperative Gemcitabine in 246 patients. Primary endpoint of the trial was OS in the ITT group (15). Interestingly, resection rate in the neoadjuvant treatment arm was only 62%. However, the resection rate in the arm receiving upfront surgery was also only 72% suggesting that in a substantial number of patients CT staging missed small metastases that prevented resection. Interestingly, the R0 resection rate was significantly higher (P<0.001) in the neoadjuvant (NA) arm with 63% compared to only 31% in the arm with upfront surgery (US). Serious adverse events were comparable in both arms (39% US, 46% NA; P=0.28). The trial missed its primary endpoint with a mOS in the UR group of 13.7 months compared to 17.1 months in the NA group (HR =0.74; P=0.074). However, when only patients were analyzed that underwent resection there was a significant benefit for the NA arm with a mOS of 29.9 months compared to 16.8 months in the UR group (P=0.001). There was also a significant improvement in the DFS in the NA group. This study shows that neoadjuvant treatment can improve the outcome of patients with resectable PDAC in a prospective setting. However, it the protocol used may not be optimal in this setting.
Another phase II/III trial from Japan that has just been presented compared upfront surgery plus adjuvant treatment with S1 with a neoadjuvant treatment with the combination of Gemcitabine plus S1 followed by surgery and adjuvant treatment with S1 (16). There were 180 patients in each arm and the primary endpoint was overall survival for the phase III part and resection rate for the phase II part. In the phase II part of the trial resection rate in the NA arm was 93% compared to 82% in the UR arm. Since the phase II part met its preplanned criteria, the phase III part was initiated. In this part of the trial neoadjuvant treatment showed a significantly better mOS compared to adjuvant treatment: 36.72 vs. 26.65 months (HR =0.72; 95% CI: 0.55–0.94; P=0.015). Also, the 2-year OS rate was improved by neoadjuvant treatment with 63.7% vs. 52.5%. The majority of the subgroups in the Forest Plot analysis benefitted from neoadjuvant treatment. Importantly, neoadjuvant Gemcitabine plus S1 did not affect operation time or operative morbidity (NA: 45.9%; NA: 49.7%). pN1 was also significantly lower in the NA arm compared to the UR arm (59.6% vs. 81.5%). Most frequently observed grade 3 or 4 adverse events were leukopenia and neutropenia in 72.8% of cases. However, these side effects did not increase perioperative mortality. Again, these data point to substantial benefit of neoadjuvant chemotherapy in patients with resectable PDAC compared to upfront resection and adjuvant treatment. The limitation of this study is that the trial only recruited Asian patients and there are so far no data on the efficacy of S1 in Caucasian patients with resectable pancreatic cancer.
Neoadjuvant treatment of resectable pancreatic cancer—standard or study?
Given the fact that we have systematic reviews and two prospective trials that show a benefit for neoadjuvant treatment of resectable PDAC one could argue that there is sufficient evidence to implement this strategy in the clinical algorithm.
However, there are still open questions that need to be addressed: What is the best neoadjuvant treatment regimen? FOLFIRINOX, modified FOLFIRNOX, Gemcitabine plus nab-Paclitaxel or other regimens, even radiochemotherapy? How much neoadjuvant treatment shall be given? 2, 3, 4 cycles? What is the role of the postoperative treatment after neoadjuvant chemotherapy? A substantial number of trials are currently underway that address these topics and will present data in due course (Table 1).
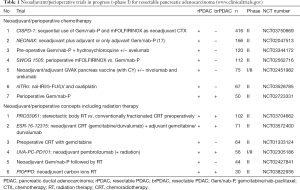
Full table
Pancreatic cancer is a highly heterogeneous disease. In a time of personalized tumor treatment, one could argue that a neoadjuvant treatment should be tailored to the individual tumor, e.g., by establishing chemotherapy specific response signatures in PDACs that could be used to predict the response of an individual tumor. There are already examples in the literature suggesting that this may be a realistic approach at least for a substantial proportion of tumors. This approach could ensure that an individual patient with a resectable PDAC receives a neoadjuvant treatment with a high chance of efficacy thereby providing the best ratio between risk by adverse effects and benefit by improving overall survival.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Conroy T, Hammel P, Hebbar M, et al. FOLFIRINOX or Gemcitabine as Adjuvant Therapy for Pancreatic Cancer. N Engl J Med 2018;379:2395-406. [Crossref] [PubMed]
- Deutsche_Krebsgesellschaft: Jahresbericht der zertifizierten Pankreaskarzinomzentren - Kennzahlenauswertung 2018. Available online: https://www.krebsgesellschaft.de/jahresberichte.html
- Assifi MM, Lu X, Eibl G, et al. Neoadjuvant therapy in pancreatic adenocarcinoma: a meta-analysis of phase II trials. Surgery 2011;150:466-73. [Crossref] [PubMed]
- Gillen S, Schuster T, Meyer Zum Büschenfelde C, et al. Preoperative/neoadjuvant therapy in pancreatic cancer: a systematic review and meta-analysis of response and resection percentages. PLoS Med 2010;7:e1000267. [Crossref] [PubMed]
- Murphy JE, Ly L, Wo JY, et al. Dose intensity of neoadjuvant FOLFIRINOX (FFX) in borderline and locally advanced pancreatic cancer (LAPC): A comparison to the adjuvant benchmark. J Clin Oncol 2019;37:392-2. [Crossref]
- Haeno H, Gonen M, Davis MB, et al. Computational modeling of pancreatic cancer reveals kinetics of metastasis suggesting optimum treatment strategies. Cell 2012;148:362-75. [Crossref] [PubMed]
- Seufferlein T. Guidelines and expert consensus in the ZfG. Z Gastroenterol 2014;52:179. [Crossref] [PubMed]
- Hewitt MJ, McPhail MJ, Possamai L, et al. EUS-guided FNA for diagnosis of solid pancreatic neoplasms: a meta-analysis. Gastrointest Endosc 2012;75:319-31. [Crossref] [PubMed]
- Hadano N, Murakami Y, Uemura K, et al. Prognostic value of circulating tumour DNA in patients undergoing curative resection for pancreatic cancer. Br J Cancer 2016;115:59-65. [Crossref] [PubMed]
- Berger AW, Schwerdel D, Reinacher-Schick A, et al. A Blood-Based Multi Marker Assay Supports the Differential Diagnosis of Early-Stage Pancreatic Cancer. Theranostics 2019;9:1280-7. [Crossref] [PubMed]
- Andriulli A, Festa V, Botteri E, et al. Neoadjuvant/preoperative gemcitabine for patients with localized pancreatic cancer: a meta-analysis of prospective studies. Ann Surg Oncol 2012;19:1644-62. [Crossref] [PubMed]
- Chun YS, Cooper HS, Cohen SJ, et al. Significance of pathologic response to preoperative therapy in pancreatic cancer. Ann Surg Oncol 2011;18:3601-7. [Crossref] [PubMed]
- de Geus SW, Evans DB, Bliss LA, et al. Neoadjuvant therapy versus upfront surgical strategies in resectable pancreatic cancer: A Markov decision analysis. Eur J Surg Oncol 2016;42:1552-60. [Crossref] [PubMed]
- Mokdad AA, Minter RM, Zhu H, et al. Neoadjuvant Therapy Followed by Resection Versus Upfront Resection for Resectable Pancreatic Cancer: A Propensity Score Matched Analysis. J Clin Oncol 2017;35:515-522. [Crossref] [PubMed]
- Tienhoven GV, Versteijne E, Suker M, et al. Preoperative chemoradiotherapy versus immediate surgery for resectable and borderline resectable pancreatic cancer (PREOPANC-1): A randomized, controlled, multicenter phase III trial. J Clin Oncol 2018;36:LBA4002. [Crossref]
- Motoi F, Kosuge T, Ueno H, et al. Randomized phase II/III trial of neoadjuvant chemotherapy with gemcitabine and S-1 versus upfront surgery for resectable pancreatic cancer (Prep-02/JSAP05). Jpn J Clin Oncol 2019;49:190-4. [Crossref] [PubMed]
- Ettrich TJ, Berger AW, Perkhofer L, et al. Neoadjuvant plus adjuvant or only adjuvant nab-paclitaxel plus gemcitabine for resectable pancreatic cancer - the NEONAX trial (AIO-PAK-0313), a prospective, randomized, controlled, phase II study of the AIO pancreatic cancer group. BMC Cancer 2018;18:1298. [Crossref] [PubMed]
Cite this article as: Seufferlein T, Ettrich TJ. Treatment of pancreatic cancer—neoadjuvant treatment in resectable pancreatic cancer (PDAC). Transl Gastroenterol Hepatol 2019;4:21.


