Palliative therapy in pancreatic cancer—interventional treatment with radiofrequency ablation/irreversible electroporation
Introduction
Pancreatic cancer (PC) still has a dismal prognosis and by 2030 PC will become the second cause of tumor-related death in USA (1). Most of patients receive a diagnosis when the tumor is unresectable. Indeed only 20% of patients have tumors that are amenable to surgery at the time of diagnosis, and LAPC accounts for 30% of the first diagnoses of PC (2). Chemotherapy is the standard of care for locally advanced pancreatic cancer (LAPC) patients (3). Intensive chemotherapy with regimens such as FOLFIRINOX (a combination of irinotecan, fluorouracil, leucovorin and oxaliplatinum) or nab-paclitaxel/Gemcitabine have proved to be able to prolong survival and to obtain promising rates of conversion surgery (4). However, despite the efforts of medical oncological therapies the rate of conversion surgery with radical resection (R0) is still low (up to 25%) (4,5). For this reason, interventional ablative treatments as emerged as a possible palliative therapy in those patients that will unlikely receive a radical resection due to the persistency of major vascular involvement, but that have not progressed towards the metastatic stage of the disease. Several types of ablative treatments have been adopted for the treatment of LAPC, such as such as radiofrequency ablation (RFA), irreversible electroporation (IRE), microwave ablation (MWA) or cryoablation. This review will provide an overview of safety and oncological results obtained so far by the two most used technique, RFA and IRE.
Interventional treatments: RFA
Introduction
RFA is a thermal technique that using a high-frequency alternating current produces tissue coagulation and protein denaturation (6). A generator is connected to a needle-electrode (rarely multiple needle-electrodes) that is inserted in the core of the tumor, producing necrosis within it and presumably, cytoreduction.
Technique
The technique is performed under ultrasound-guidance. Bubbles are produced during the heat of the tissue and they are clearly visible, thus the ultrasound live control is of paramount importance to control the amount of the treated area. If necessary, multiple passages can be performed for bigger tumors.
In most of the studies published RFA is performed using a traditional laparotomic approach (7-9). Recently, the technique has been adopted with a mini-invasive approach, percutaneously or endoscopically (10,11). The possibility to use a mini invasive approach is important to reduce the surgical stress of the laparotomy, the length of stay, maintaining encouraging results in terms of safety.
Indications
RFA should be used only for LAPC already treated with medical oncological treatment and never upfront. At the time of re-staging after 3 to 6 months (or more) or systemic therapy the patient is evaluated in a multidisciplinary scenario, involving oncologists, interventional radiologists and surgeons. If the tumor shows no signs of radiological, laboratoristic (e.g., increase of Ca 19-9 levels) or clinical progression then RFA may be considered as a palliative therapeutic option.
The best LAPC to treat with RFA is a mass-forming PC, located at the body of the gland, where the percutaneous approach can be used (10). Whilst for LAPC of the head of the gland, the endoscopic one seems to be promising (11).
Oncological results
The oncological results of RFA are still controversial. Our group has already provided in the past encouraging results in terms of overall survival (OS), that reached up to 34 months when RFA was associated with multiple other therapies (namely radiochemotherapy and intra-arterial and systemic chemotherapy) (7,12). It must be noted that the series published by our group come mostly from retrospective cohorts and patients may overlap, demonstrating selection and population biases. Our group has published a retrospective series of 30 LAPC patients in whom the SMAD4 gene was tested. The analysis of this gene seems to be able to predict the likely growth of the tumor, if local or systemic (13). In this series we found that patients with a wild-type gene were more prone to benefit from RFA, than those with a mutated gene (14). Furthermore, the analysis of SMAD4 is cheap, not time-consuming and it might be done at the time of diagnosis. It is likely that this strategy might help to select LAPC with a tendency to a local growth, where RFA (or other ablative treatments) might play an efficacious role to obtain the local control of the disease. However, further prospective studies are needed to validate our findings.
Complications
The major problem of RFA is its thermal nature. Heat spread can produce a damage of the peripancreatic surrounding structures, that in a LAPC are mostly vascular structures. This aspect is responsible for possible severe adverse events, so that morbidity and mortality rates range from 0% to 3% and from 0% to 28%, respectively (15). Hemorrhages, pancreatic fistula, biliary or duodenal burn and vein thrombosis are the most commonly reported (15,16). The management of this complications might be difficult, so RFA should always be adopted by very specialized centers in pancreatic surgery. In this field, the presence of uncovered metal stents is an absolute contraindication for the treatment of LAPC of the head of the gland, as the conductive capacity of the metal might facilitate the spread of the heat to surrounding structures, increasing the possibility of even serious adverse events to the biliary tree or the duodenum.
Follow-up
At our institution, we perform the first cross-sectional imaging 30 days after RFA, where a “hole” can be seen as result of the tumor necrosis produced (10,11,17). Before this time, imaging should be done to rule out possible complications, rather than to detect any efficacy of the procedure. Interestingly, some patients experience a reduction of the pre-procedure levels of RFA of Ca 19-9, a sort of indirect demonstration of the cytoreduction induced (18). The fact that some other patients do not experience this demonstrates that further data are needed to clarify the effective cytoreductive role of RFA.
Immune stimulation
Virtually all ablative treatments are able to elicitate an almost specific anti-tumor immune response. Briefly, once the tumor cell dies it release in the bloodstream some peculiar antigens that, at the end, will stimulate the immune system to react against the cancer (19). In a clinical setting this has never been demonstrated. Our group has already demonstrated some kind of immunomodulation after the laparotomic application of RFA on PC. It seems that RFA is able to delay the immunoregulation of the immune response (20). However, this study has some inherent bias and it should be considered as a starting point for further investigations.
Interventional treatments: IRE
Introduction
Starting from the settings adopted on electrochemotherapy (namely reversible electroporation) to create nanopores in the cell membrane, in 2005 Davalos et al. developed a mathematical model to irreversibly create a permeabilization of the cell membrane. Thus, the Authors realized the irreversible form of electroporation (IRE), claiming it as a new valid technique to ablate substantial volumes of tumor (21). From that moment on, IRE was applied in surgical oncology to treat solid tumors for whom the radical resection was not possible.
Technique
The technique has been applied on several solid tumors and in 2012 Martin et al. published the first experience on PC (22). IRE was at first applied intraoperatively using a laparotomic approach. In general, multiple needle-electrodes connected to a generator of current are placed in and around the tumor. According to specific settings, local electric fields are creates so that an irreversible permeabilization of the cell membrane is produced. This event will ultimately lead to the death of the cell, preserving the underlying matrix, the vessels and the biliary structures possibly included in the ablation area (21,23,24). The technique has been widely described by Martin et al. (25) and in 2016 a consensus was reached to establish the settings to adopt universally, in order to homogenize the methods and to compare the results (26). The laparotomic approach is the most adopted one (22,25,27-30), however there are several reports on the use of IRE using a laparoscopic (28) or a percutaneous one (31-36). Anyway, the technique needs a proper preoperative planning, calculating the target and the ablation volume, according to tumor geometry. However, it seems that, despite all theoretical efforts, a misestimation of the ablated volume might happen (in excess) (37).
Indications
A therapeutic algorithm has been already proposed by the pioneers of IRE on PC (25). Briefly, the patient has already been received a systemic therapy for LAPC and the disease has not been progressed either locally or systemically. Staging and re-staging are based on clinical conditions, performance status, imaging and Ca 19-9 levels. While for RFA the best LAPC to treat is a mass-forming one, using IRE, instead, all possible tumor shapes can be treated, even when the tumor encase the peripancreatic vessels. There is a theoretical dimensional cut-off for IRE that is 4 cm, hence greater tumors should not be treated. IRE is more easily performed intraoperatively using a laparotomic approach, under ultrasound-guidance. However, it can be done percutaneously, even skilled interventional radiologists are needed. The presence of a metal stent is not an absolute contraindication for LAPC of the head of the pancreas, since IRE is not a thermal ablative technique. However, the metal might create an electric fields distortion electric fields produced, preventing IRE from being effective in producing the ablation area planned (38,39), or even exposing patients to severe complications (40). When needed, the use of covered metal stent might help to reduce the risk of ineffective ablation or adverse events (26).
Oncological results
The oncological results of IRE seems to be promising, with median OS from diagnosis or even treatment of 27 months (35,36). Very recently, some eastern authors report an impressive OS of 28 months when IRE was followed by 3 months of TS-1 regimen of chemotherapy (Tegafur, Gimeracil and Oteracil) (41). However, other studies report worse prognosis, around 15–17 months (27,34,42). It is presumable that the design of the studies, and, more probably, the expertise of the users are two important factors that can impact even on the oncological results. Notably, the most frequently reported results on OS are close to those reported in a recent patient-level meta-analysis of LAPC patients treated with FOLFIRINOX as first-line treatment (median OS of 24.2 months) (4). Table 1 shows the list of the most representative studies published so far about the use of IRE on LAPC.
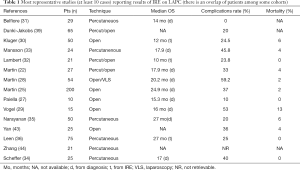
Full table
Complications
Despite its non-thermal nature, some complications may occur after IRE and the list of possible adverse events entails a heterogeneous number of complications, such as pancreatic fistula, venous and arterial thrombosis, pseudoaneurysm or pancreatic abscess (16,45). The morbidity rate can reach up to 30% and the morbidity is not nil (15). These number highlights the importance of the learning curve and the need to adopt IRE only in specialized centers.
Imaging
One of the most controversial topics about the use of IRE on PC is how to interpret post-procedural imaging. The radiological findings can be divided into tumorous and non-tumorous. Schulz et al. found that within 30 days of IRE a multi-phase contrast-enhanced CT-scan (ceCT) of the abdomen is not useful and, in order to detect non-tumorous findings, it should be done within 15 days of IRE. In this sense, frequent findings were abdominal wall edema or ascites, with no clinical impact, or even gastrointestinal hemorrhage, portal vein thrombosis or bowel perforation with clear clinical impact (46). The effect of IRE on vessel wall is still debated, as some authors report a narrowing/compression (46), but some others do not (47).
The tumorous findings are heterogeneous, as immediately after IRE the ablation zone might be bigger than expected and hypodense. This will solve with time as edema and hyperemia, reduce and scar tissue takes place. If a lesion is stable for a long, and then increase in volume and contrast enhancement are appreciated afterwards, then concerns about a possible local recurrence should be paid.
Post-IRE magnetic resonance imaging (MRI) findings have been investigated too. Vroomen et al. found that most of the treated LAPC revealed absent or decreased contrast enhancement, with a typical hyperintense rim on ceMRI. Even at ceMRI the ablation volume increases in the early phases (the first 6 weeks) and then decreases (48). This finding should be considered and integrated with other data (increase of Ca 19-9 levels), to detect any early local recurrence of the disease.
In general, for IRE, as well as for RFA, both RECIST (49) and mRECIST (50) criteria do not seem adequate to assess the effects of the ablation on PC.
Immune stimulation
The type of cell death caused by IRE is apoptosis (51). Thus, it is reasonable that the tumor antigens are more intact than those produced with the necrosis caused by RFA. In 2007, Al-Sakere et al. found in preclinical models that IRE does not elicitate an immune response (52). However, opposite results came afterwards from studies on animal models, that claimed that IRE can trigger the immune response, even stronger than RFA in this sense (53). Furthermore, recently Lin et al. discovered that the combination of IRE and allogeneic NK cell played a synergistic effect, enhancing the immune function of patients demonstrating a fruitful post-IRE immunomodulation that can amplify systemically the results obtained locally (54). These controversial results rely on the complex interaction between the immune system and PC (55). A project on mouse models of PC treated with RFA and IRE is running at our Institution.
Conclusions
The treatment of LAPC is still a challenge. Only a small percentage of LAPC patients will be surgically explored and only a minority will receive a radical resection. The vast majority will still continue to receive various lines of chemotherapy, variously associated with radiotherapy, according to the natural history of the tumor, to the clinical conditions and to the possible side effects of the systemic treatments. A subgroup of LAPC will never undergo surgery as the tumor will not shrink nor downstage after systemic therapies. For these LAPC a valid palliative option might be to perform interventional treatments, such as RFA and IRE. These techniques would help to obtain a local control of the disease and they must be chosen within multidisciplinary decisions. The aim of RFA and IRE is to offer a palliative treatment, possibly with a mini-invasive approach, to LAPC patients with a good performance status, that have already been treated with a consolidative systemic therapy. Considering the possible complications, even serious, of whom they might be cause of, they should be adopted only by expert users in specialized centers of interventional pancreatology. The selection of LAPC to treat is of paramount importance, as mass-forming ones might be safely treated with RFA, while those still entailing major peripancreatic vessels might benefit from a treatment with IRE.
Finally, further studies will be necessary to clarify whether RFA and IRE might be used to boost the immune system to react against PC.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Rahib L, Smith BD, Aizenberg R, et al. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res 2014;74:2913-21. [Crossref] [PubMed]
- Gurusamy KS, Kumar S, Davidson BR, et al. Resection versus other treatments for locally advanced pancreatic cancer. Cochrane Database Syst Rev 2014. [PubMed]
- Tempero MA, Malafa MP, Al-Hawary M, et al. Pancreatic Adenocarcinoma, Version 2.2017, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw 2017;15:1028-61. [Crossref] [PubMed]
- Suker M, Beumer BR, Sadot E, et al. FOLFIRINOX for locally advanced pancreatic cancer: a systematic review and patient-level meta-analysis. Lancet Oncol 2016;17:801-10. [Crossref] [PubMed]
- Hammel P, Lacy J, Portales F, et al. Phase II LAPACT trial of nab-paclitaxel (nab-P) plus gemcitabine (G) for patients with locally advanced pancreatic cancer (LAPC). J Clin Oncol 2018;36:204.
- Ahmed M, Brace CL, Lee FT Jr, et al. Principles of and advances in percutaneous ablation. Radiology 2011;258:351-69. [Crossref] [PubMed]
- Cantore M, Girelli R, Mambrini A, et al. Combined modality treatment for patients with locally advanced pancreatic adenocarcinoma. Br J Surg 2012;99:1083-8. [Crossref] [PubMed]
- Girelli R, Frigerio I, Salvia R, et al. Feasibility and safety of radiofrequency ablation for locally advanced pancreatic cancer. Br J Surg 2010;97:220-5. [Crossref] [PubMed]
- Girelli R, Frigerio I, Giardino A, et al. Results of 100 pancreatic radiofrequency ablations in the context of a multimodal strategy for stage III ductal adenocarcinoma. Langenbecks Arch Surg 2013;398:63-9. [Crossref] [PubMed]
- D'Onofrio M, Crosara S, De Robertis R, et al. Percutaneous Radiofrequency Ablation of Unresectable Locally Advanced Pancreatic Cancer: Preliminary Results. Technol Cancer Res Treat 2017;16:285-94. [Crossref] [PubMed]
- Crino SF, D'Onofrio M, Bernardoni L, et al. EUS-guided Radiofrequency Ablation (EUS-RFA) of Solid Pancreatic Neoplasm Using an 18-gauge Needle Electrode: Feasibility, Safety, and Technical Success. J Gastrointestin Liver Dis 2018;27:67-72. [PubMed]
- Giardino A, Girelli R, Frigerio I, et al. Triple approach strategy for patients with locally advanced pancreatic carcinoma. HPB (Oxford) 2013;15:623-7. [Crossref] [PubMed]
- Iacobuzio-Donahue CA, Fu B, Yachida S, et al. DPC4 gene status of the primary carcinoma correlates with patterns of failure in patients with pancreatic cancer. J Clin Oncol 2009;27:1806-13. [Crossref] [PubMed]
- Paiella S, Malleo G, Cataldo I, et al. Radiofrequency ablation for locally advanced pancreatic cancer: SMAD4 analysis segregates a responsive subgroup of patients. Langenbecks Arch Surg 2018;403:213-20. [PubMed]
- Ruarus A, Vroomen L, Puijk R, et al. Locally Advanced Pancreatic Cancer: A Review of Local Ablative Therapies. Cancers (Basel) 2018.10. [PubMed]
- Nundy S, Gouma Dirk J, Oxford University P. Complications after gastrointestinal surgery. New Delhi: Oxford University Press, 2017.
- Paiella S, Salvia R, Ramera M, et al. Local Ablative Strategies for Ductal Pancreatic Cancer (Radiofrequency Ablation, Irreversible Electroporation): A Review. Gastroenterol Res Pract 2016;2016. [Crossref] [PubMed]
- D'Onofrio M, Barbi E, Girelli R, et al. Variation of tumoral marker after radiofrequency ablation of pancreatic adenocarcinoma. J Gastrointest Oncol 2016;7:213-20. [PubMed]
- Chu KF, Dupuy DE. Thermal ablation of tumours: biological mechanisms and advances in therapy. Nat Rev Cancer 2014;14:199-208. [Crossref] [PubMed]
- Giardino A, Innamorati G, Ugel S, et al. Immunomodulation after radiofrequency ablation of locally advanced pancreatic cancer by monitoring the immune response in 10 patients. Pancreatology 2017;17:962-6. [Crossref] [PubMed]
- Davalos RV, Mir LM, Rubinsky B. Tissue Ablation with Irreversible Electroporation. Ann Biomed Eng 2005;33:223. [Crossref] [PubMed]
- Martin RC 2nd, McFarland K, Ellis S, et al. Irreversible electroporation therapy in the management of locally advanced pancreatic adenocarcinoma. J Am Coll Surg 2012;215:361-9. [Crossref] [PubMed]
- Al-Sakere B, Andre F, Bernat C, et al. Tumor ablation with irreversible electroporation. PLoS One 2007;2. [Crossref] [PubMed]
- Rubinsky B, Onik G, Mikus P. Irreversible electroporation: a new ablation modality--clinical implications. Technol Cancer Res Treat 2007;6:37-48. [Crossref] [PubMed]
- Martin RC 2nd, Kwon D, Chalikonda S, et al. Treatment of 200 locally advanced (stage III) pancreatic adenocarcinoma patients with irreversible electroporation: safety and efficacy. Ann Surg 2015;262:486-94; discussion 92-4. [Crossref] [PubMed]
- Martin RC 2nd, Durham AN, Besselink MG, et al. Irreversible electroporation in locally advanced pancreatic cancer: A call for standardization of energy delivery. J Surg Oncol 2016;114:865-71. [Crossref] [PubMed]
- Paiella S, Butturini G, Frigerio I, et al. Safety and feasibility of Irreversible Electroporation (IRE) in patients with locally advanced pancreatic cancer: results of a prospective study. Dig Surg 2015;32:90-7. [Crossref] [PubMed]
- Martin RC 2nd, McFarland K, Ellis S, et al. Irreversible electroporation in locally advanced pancreatic cancer: potential improved overall survival. Ann Surg Oncol 2013;20 Suppl 3:S443-9. [Crossref] [PubMed]
- Vogel JA, Rombouts SJ, de Rooij T, et al. Induction Chemotherapy Followed by Resection or Irreversible Electroporation in Locally Advanced Pancreatic Cancer (IMPALA): A Prospective Cohort Study. Ann Surg Oncol 2017;24:2734-43. [Crossref] [PubMed]
- Kluger MD, Epelboym I, Schrope BA, et al. Single-Institution Experience with Irreversible Electroporation for T4 Pancreatic Cancer: First 50 Patients. Ann Surg Oncol 2016;23:1736-43. [Crossref] [PubMed]
- Belfiore G, Belfiore MP, Reginelli A, et al. Concurrent chemotherapy alone versus irreversible electroporation followed by chemotherapy on survival in patients with locally advanced pancreatic cancer. Med Oncol 2017;34:38. [Crossref] [PubMed]
- Lambert L, Horejs J, Krska Z, et al. Treatment of locally advanced pancreatic cancer by percutaneous and intraoperative irreversible electroporation: general hospital cancer center experience. Neoplasma 2016;63:269-73. [PubMed]
- Mansson C, Brahmstaedt R, Nilsson A, et al. Percutaneous irreversible electroporation for treatment of locally advanced pancreatic cancer following chemotherapy or radiochemotherapy. Eur J Surg Oncol 2016;42:1401-6. [Crossref] [PubMed]
- Scheffer HJ, Vroomen LG, de Jong MC, et al. Ablation of Locally Advanced Pancreatic Cancer with Percutaneous Irreversible Electroporation: Results of the Phase I/II PANFIRE Study. Radiology 2017;282:585-97. [Crossref] [PubMed]
- Narayanan G, Hosein PJ, Beulaygue IC, et al. Percutaneous Image-Guided Irreversible Electroporation for the Treatment of Unresectable, Locally Advanced Pancreatic Adenocarcinoma. J Vasc Interv Radiol 2017;28:342-8. [Crossref] [PubMed]
- Leen E, Picard J, Stebbing J, et al. Percutaneous irreversible electroporation with systemic treatment for locally advanced pancreatic adenocarcinoma. J Gastrointest Oncol 2018;9:275-81. [Crossref] [PubMed]
- Bhutiani N, Doughtie CA, Martin RC 2nd. Ultrasound validation of mathematically modeled irreversible electroporation ablation areas. Surgery 2016;159:1032-40. [Crossref] [PubMed]
- Dunki-Jacobs EM, Philips P, Martin RC 2nd. Evaluation of thermal injury to liver, pancreas and kidney during irreversible electroporation in an in vivo experimental model. Br J Surg 2014;101:1113-21. [Crossref] [PubMed]
- Dunki-Jacobs EM, Philips P, Martin RC 2nd. Evaluation of resistance as a measure of successful tumor ablation during irreversible electroporation of the pancreas. J Am Coll Surg 2014;218:179-87. [Crossref] [PubMed]
- Mansson C, Nilsson A, Karlson BM. Severe complications with irreversible electroporation of the pancreas in the presence of a metallic stent: a warning of a procedure that never should be performed. Acta Radiol Short Rep 2014;3. [Crossref] [PubMed]
- Huang KW, Yang PC, Pua U, et al. The efficacy of combination of induction chemotherapy and irreversible electroporation ablation for patients with locally advanced pancreatic adenocarcinoma. J Surg Oncol 2018;118:31-6. [Crossref] [PubMed]
- Vogl TJ, Panahi B, Albrecht MH, et al. Microwave ablation of pancreatic tumors. Minim Invasive Ther Allied Technol 2018;27:33-40. [Crossref] [PubMed]
- Yan L, Chen YL, Su M, et al. A Single-institution Experience with Open Irreversible Electroporation for Locally Advanced Pancreatic Carcinoma. Chin Med J (Engl) 2016;129:2920-5. [Crossref] [PubMed]
- Zhang Y, Shi J, Zeng J, et al. Percutaneous Irreversible Electroporation for Ablation of Locally Advanced Pancreatic Cancer: Experience From a Chinese Institution. Pancreas 2017;46:e12-4. [Crossref] [PubMed]
- Martin RC 2nd. Multi-disciplinary management of locally advanced pancreatic cancer with irreversible electroporation. J Surg Oncol 2017;116:35-45. [Crossref] [PubMed]
- Schulz B, Ou J, Van Meter T, et al. Early nontumorous CT findings after irreversible electroporation of locally advanced pancreatic cancer. Abdom Radiol (NY) 2016;41:2142-9. [Crossref] [PubMed]
- Gonzalez-Beicos A, Venkat S, Songrug T, et al. Irreversible Electroporation of Hepatic and Pancreatic Malignancies: Radiologic-Pathologic Correlation. Tech Vasc Interv Radiol 2015;18:176-82. [Crossref] [PubMed]
- Vroomen L, Scheffer HJ, Melenhorst M, et al. MR and CT imaging characteristics and ablation zone volumetry of locally advanced pancreatic cancer treated with irreversible electroporation. Eur Radiol 2017;27:2521-31. [Crossref] [PubMed]
- Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 2009;45:228-47. [Crossref] [PubMed]
- Lencioni R, Llovet JM. Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin Liver Dis 2010;30:52-60. [Crossref] [PubMed]
- Zhang Z, Li W, Procissi D, et al. Rapid dramatic alterations to the tumor microstructure in pancreatic cancer following irreversible electroporation ablation. Nanomedicine (Lond) 2014;9:1181-92. [Crossref] [PubMed]
- Al-Sakere B, Bernat C, Andre F, et al. A study of the immunological response to tumor ablation with irreversible electroporation. Technol Cancer Res Treat 2007;6:301-6. [Crossref] [PubMed]
- Bulvik BE, Rozenblum N, Gourevich S, et al. Irreversible Electroporation versus Radiofrequency Ablation: A Comparison of Local and Systemic Effects in a Small-Animal Model. Radiology 2016;280:413-24. [Crossref] [PubMed]
- Lin M, Alnaggar M, Liang S, et al. An important discovery on combination of irreversible electroporation and allogeneic natural killer cell immunotherapy for unresectable pancreatic cancer. Oncotarget 2017;8:101795-807. [Crossref] [PubMed]
- Sideras K, Braat H, Kwekkeboom J, et al. Role of the immune system in pancreatic cancer progression and immune modulating treatment strategies. Cancer Treat Rev 2014;40:513-22. [Crossref] [PubMed]
Cite this article as: Paiella S, De Pastena M, D’Onofrio M, Crinò SF, Pan TL, De Robertis R, Elio G, Martone E, Bassi C, Salvia R. Palliative therapy in pancreatic cancer—interventional treatment with radiofrequency ablation/irreversible electroporation. Transl Gastroenterol Hepatol 2018;3:80.


