A learning curve for laparoscopic liver resection: an effective training system and standardization of technique
Introduction
Liver resection has historically been associated with high morbidity and mortality rates, however, the advancement of surgical techniques and peri-operative management enable liver resection to become the most effective and commonly used operation. Laparoscopic liver resection (LHx) is a relatively new surgical technique, the use of which has been increasing with more than 9,500 cases worldwide (1,2). Compared to the open liver resection (Hx), LHx has some advantages such as: a smaller incision; less blood loss; decreased post-operative morbidity; and a shorter length of stay in hospital (3,4). Furthermore, recent studies report that LHx was associated with long-term outcomes compared with those of open Hx (5-7). However, the worldwide increase of LHx has been still hindered for the following reasons: the fear of intraoperative bleeding of major vessels, difficulties in location of liver tumor and enough oncological surgical margins (8,9). Therefore, information regarding the learning curve associated with LHx seemed to be necessary especially for a center where not many operations of this nature are performed.
A learning curve is defined as “the improvement in performance over time, or the change in the ability to complete a task until failure is reduced to a constant acceptable rate” (10). Outcomes relating to a surgeon’s learning curve include intra-operative measures of efficiency and proficiency such as operative duration, blood loss, or conversion rate, as well as patient-centered outcomes such as: morbidity; mortality; transfusion rate; intensive care unit (ICU) days; and overall length of stay in hospital.
In this study, a literature review of published research which included a learning curve for LHx was performed. Moreover, a new step-wise training method for inexperienced surgeons and a standardization of a technique for LHx at the Tokushima University Hospital, focusing especially on laparoscopic left hepatectomy (LLHx), was proposed.
Learning curve for LHx
There have been several reports from single centers regarding LHx (Table 1). Vigano et al. (11) reported a learning curve by a cumulative sum (CUSUM) analysis of conversions for the first time. They claimed that LHx was categorized in specialized hepato-pancreatic-biliary operations, and 60 procedures were necessary to reach the cut-off point of a minimal conversion rate. In other words, after 60 cases, the conversion rate reached the average value for the entire cohort and only further improved from that point on. Cai et al. (12) showed learning curve for 4 different well-defined LHx procedures in a single center experience. Fifteen to thirty cases for left hemihepatectomy; 43 cases for left lateral sectionectomy; 35 cases for non-anatomic liver resection were necessary. Twenty-eight segmentectomies as the numbers of procedures were needed to reach the best peri-operative results. Nomi et al. (10) reported that 45 laparoscopic major Hx procedures were required for reducing operating time. Lin et al. (13) investigated the learning curve of operating time, blood loss and perioperative complication rate, and reported that 22 cases were required to achieve the learning curve of minor LHx. Furthermore, they recommended that advanced LHx (LHx for tumors in difficult locations and major Hx) should be introduced after their 60th case. Hasegawa et al. (14) showed that to obtain a low morbidity rate, 60 laparoscopic minor Hx could provide adequate experience before the introduction of laparoscopic major Hx. The published evidence has focused on a single center experience, often represented by different surgeons and/or based on few procedures. On the other hand, Tomassini et al. (15) evaluated the single-surgeon learning curve for LHx over an 11 year period. They concluded that at least 160 cases were needed to complete the single-surgeon learning curve for performing different types of LHx safely. A minimum of 50 cases could provide a significant decrease in blood loss.
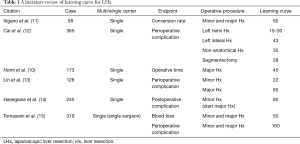
Full table
Method for the step-wise training of inexperienced surgeons
In order to achieve a safer LHx, a step-wise training method was developed at the Tokushima University Hospital to educate inexperienced surgeons how to do a standardized procedure.
Training using a dry box
First step is a training in basic techniques with a dry box and checked by senior surgeons. The tasks were classified into six [6] levels of difficulty. The inexperienced surgeons recorded the number of times, and a chair person of department checked when the trainee was ready for the next step.
Pre-operative three-dimensional (3D) simulation
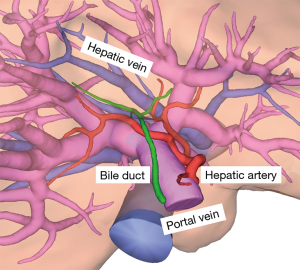
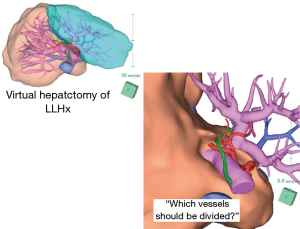
Second step was pre-operative simulation with a 3D simulation imaging system for each patient. The 3D simulation imaging system, the Synapse Vincent (Fuji Film, Tokyo, Japan), revealed all vessels including hepatic artery, portal vein, hepatic vein and bile duct respectively (Figure 1). The authors have already reported that preoperative 3D imaging could achieve both precise volumetry and the confirmation of hilar anatomy in one-time examination (16). Inexperienced surgeons must perform “virtual hepatectomy”, by themselves, including deciding when and which vessels should be divided during parenchymal dissection (Figure 2).
Self and mentor assessment
Third was a self-assessment of actual surgical technique and understanding of anatomy and a feedback from both senior surgeons and a chair person of department. There is a check-sheet of both surgical techniques and non-technical skill. Inexperienced and senior surgeons write that check-sheet. Finally, a chair person gives the inexperienced surgeons further feedback.
Standardized LLHx procedure
The left lobe mobilization and the taping of hepatoduodenal ligament was performed laparoscopically, following which a small incision (about 7 cm long) was made. The left Glissonean pedicle were encircled for inflow control, in some cases, completion of encirclement of the left Glissonean pedicle was performed laparoscopically. After division of the Arantius’ ligament, a space between the left Glissonean pedicle and the liver parenchyma made by retracting the caudal stump of the ligament was used to encircle the left Glissonean pedicle (17). Common trunk of the middle and left hepatic vein were encircled for outflow control. Then, cotton tape for a hanging maneuver was pass though on the ventral side of the inferior vena cava. A pure Lap-LHx could be performed once these procedures had been mastered.
Discussion
The incidence of LHx has been increased in the past decade. There have been some reports about some advantages of LHx, in both short and long-term outcomes after operation. The use of a minor LHx was regarded as a standard surgical practice in the Second International Consensus Conference on LHx. However, the procedure has been still in the assessment phase and a major LHx still remains in the exploration phase since its risks have not been fully understood. Extending the indications for LHx must be carefully decided. From a literature review of published studies of a learning curve for LHx, it was suggested that 20 to 40 cases were necessary for a minor Hx, and 40 to 60 cases for a major Hx. However, this depended on individual institutions.
It has been recently reported that both training using a surgical box model in laparoscopic surgery and a virtual training are effective for inexperienced surgeons (18-20). Surgical training is obviously necessary for inexperienced surgeons to obtain a safe operative technique for LHx. Furthermore, such a high-quality training may lead to a minimum learning curve for LHx. All three steps including dry box training, 3D simulation, and an assessment—feedback system are all critical components. Inexperienced surgeons have to perform pre-operative simulations for all patients with Hx, regardless of whether the procedure is laparoscopic or open in Tokushima University Hospital. In addition to surgical training, a standardization of a technique for LHx is also important for a learning curve. Inexperienced surgeons will be confused if operative techniques or procedures change depending on the senior surgeons. The published evidence for a learning curve has focused on a single center experience, often represented by different surgeons and/or based on few procedures. It is considered critical to train repeatedly, sharing common operative procedures.
In conclusion, the step-wise training and standardized procedure for LHx described in this study enabled inexperienced surgeons to perform a LHx confidently and safely. Furthermore, such a construction of a training system might lead to a minimal learning curve for LHx though further investigations are necessary.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Wakabayashi G, Cherqui D, Geller DA, et al. Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg 2015;261:619-29. [PubMed]
- Nguyen KT, Gamblin TC, Geller DA. World review of laparoscopic liver resection-2,804 patients. Ann Surg 2009;250:831-41. [Crossref] [PubMed]
- Ciria R, Cherqui D, Geller DA, et al. Comparative short term benefits of laparoscopic liver resection: 9,000 cases and climbing. Ann Surg 2016;263:761-77. [Crossref] [PubMed]
- Nguyen KT, Marsh JW, Tsung A, et al. Comparative benefits of laparoscopic vs open hepatic resection: a critical appraisal. Arch Surg 2011;146:348-56. [Crossref] [PubMed]
- Geller DA, Tsung A. Long-term outcomes and safety of laparoscopic liver resection surgery for hepatocellular carcinoma and metastatic colorectal cancer. J Hepatobiliary Pancreat Sci 2015;22:728-30. [Crossref] [PubMed]
- Beppu T, Wakabayashi G, Hasegawa K, et al. Long-term and perioperative outcomes of laparoscopic versus open liver resection for colorectal liver metastases with propensity score matching: a multi-institutional Japanese study. J Hepatobiliary Pancreat Sci 2015;22:711-20. [Crossref] [PubMed]
- Hasegawa Y, Nitta H, Sasaki A, et al. Long-term outcomes of laparoscopic versus open liver resection for liver metastases from colorectal cancer: a comparative analysis of 168 consecutive cases at a single center. Surgery 2015;157:1065-72. [Crossref] [PubMed]
- Soubrane O, Schwarz L, Cauchy F, et al. A conceptual technique for laparoscopic right hepatectomy based on facts and oncologic principles: the caudal approach. Ann Surg 2015;261:1226-31. [Crossref] [PubMed]
- Rethy A, Langø T, Mårvik R. Laparoscopic ultrasound for hepatocellular carcinoma and colorectal liver metastasis: an overview. Surg Laparosc Endosc Percutan Tech 2013;23:135-44. [Crossref] [PubMed]
- Nomi T, Fuks D, Kawaguchi Y, et al. Learning curve for laparoscopic major hepatectomy. Br J Surg 2015;102:796-804. [Crossref] [PubMed]
- Vigano L, Laurent A, Tayar C, et al. The learning curve in laparoscopic liver resection: improved feasibility and reproducibility. Ann Surg 2009;250:772-82. [Crossref] [PubMed]
- Cai X, Li Z, Zhang Y, et al. Laparoscopic liver resection and the learning curve: a 14-year, single-center experience. Surg Endosc 2014;28:1334-41. [Crossref] [PubMed]
- Lin CW, Tsai TJ, Cheng TY, et al. The learning curve of laparoscopic liver resection after the Louisville statement 2008: Will it be more effective and smooth? Surg Endosc 2016;30:2895-903. [Crossref] [PubMed]
- Hasegawa Y, Nitta H, Takahara T, et al. Safely extending the indications of laparoscopic liver resection: When should we start laparoscopic major hepatectomy? Surg Endosc 2017;31:309-16. [Crossref] [PubMed]
- Tomassini F, Scuderi V, Colman R, et al. The single surgeon learning curve of laparoscopic liver resection: A continuous evolving process through stepwise difficulties. Medicine (Baltimore) 2016;95. [Crossref] [PubMed]
- Enkhbold Ch, Shimada M, Utsunomiya T, et al. One-stop shop for 3-dimensional anatomy of hepatic vasculature and bile duct with special reference to biliary image reconstruction. Hepatogastroenterology 2013;60:1861-4. [PubMed]
- Cho A, Yamamoto H, Kainuma O, et al. Arantius’ ligament approach for the left extrahepatic Glissonean pedicle in pure laparoscopic left hemihepatectomy. Asian J Endosc Surg 2012;5:187-90. [Crossref] [PubMed]
- De Win G, Van Bruwaene S, Allen C, et al. Design and implementation of a proficiency-based, structured endoscopy course for medical students applying for a surgical specialty. Adv Med Educ Pract 2013;4:103-15. [Crossref] [PubMed]
- McDougall EM, Kolla SB, Santos RT, et al. Preliminary study of virtual reality and model simulation for learning laparoscopic suturing skills. J Urol 2009;182:1018-25. [Crossref] [PubMed]
- Botden SM, Torab F, Buzink SN, et al. The importance of haptic feedback in laparoscopic suturing training and the additive value of virtual reality simulation. Surg Endosc 2008;22:1214-22. [Crossref] [PubMed]
Cite this article as: Saito Y, Yamada S, Imura S, Morine Y, Ikemoto T, Iwahashi S, Shimada M. A learning curve for laparoscopic liver resection: an effective training system and standardization of technique. Transl Gastroenterol Hepatol 2018;3:45.


