Prophylactic antibiotics at the time of elective cholecystectomy are effective in reducing the post-operative infective complications: a systematic review and meta-analysis
Introduction
The most frequent complication in patients undergoing cholecystectomy is surgical site infection (SSI) (1). The direct costs of SSI is due to prolonged hospitalization, re-admissions, frequent visits in the outpatient department and/or emergency visits, additional surgical procedures, and antibiotics therapy for an extended time period. Furthermore, the list of supplementary direct costs may continue to rise from the compulsory radiological procedures, laboratory investigations, frequent visits of health-care community workers at home, other ancillary services, and specialized levies. Indirect economic burden of SSI is very challenging to measure which may include lost productivity of the patient, a temporary or permanent decline in physical, reduction in the functional or mental capacity of the patient and reduced health-related quality of life (2-6). Since the introduction of laparoscopic cholecystectomy for the management of benign gallbladder disorders, it has undergone several innovative and dramatic changes. Although minimal invasive surgery for gallbladder surgery has offered several advantages due to reduced tissue handling and tissue trauma but prophylactic use of antibiotics to prevent SSI has not altered. In laparoscopic cholecystectomy the incisions are smaller compared to open cholecystectomy, and the wounds are not directly exposed to microbiological contamination of operative filed because all manipulations of the excised organ are made through a trocar that isolates the surgical wound. Therefore, contemporary clinical trials started focusing on the re-evaluation of the practicality of antibiotic prophylaxis in elective laparoscopic cholecystectomy (ELC). The meta-analyses (7-10) of randomized, controlled trials investigating the beneficial and harmful effects of prophylactic antibiotics to prevent SSI in patients undergoing ELC, failed to demonstrate advantages of antibiotics in term of SSI but horizon of overall postoperative complications and distant infective complications was over-sighted either intentionally or un-intentionally. The purpose of this meta-analysis is to re-visit the published evidence and attempt to generate latest evidence whether prophylactic antibiotics reduce the incidence of SSI as well as all types of post-operative infective complications.
Methods
Electronic data base search
Medline (via PubMed), Embase, Scopus, Cochrane Colorectal Cancer Group (CCCG) Controlled Trial Register, the Cochrane Central Register of Controlled Trials (CENTRAL) in the Cochrane Library and Science Citation Index Expanded were explored until March 2018 to find relevant published RCTs. The search terms were constructed based on patients, interventions/comparators, and outcomes as follows:
The MeSH terms related to the gall stones, cholecystectomy and prophylactic intravenous antibiotics were identified from the PubMed and subsequently inserted in the search boxes of other electronic databases. Attempts to find extra trials were also made by the hand searching of the references of published studies.
- Patients: all patients with cholecystitis, cholelithiasis, gallstones.
- Intervention/comparator: intravenous antibiotics at the time of induction.
- Outcomes: length of stay in hospital, all infective complications, superficial SSI, deep SSI, distant infections and deep space infection.
The MeSH terms related to the gall stones, cholecystectomy and prophylactic intravenous antibiotics were identified from the PubMed and subsequently inserted in the search boxes of other electronic databases. Attempts to find extra trials were also made by the hand searching of the references of published studies.
Data management
Two reviewers (MSS, JB) independently searched and selected studies and disagreements were resolved by consensus. Inclusion criteria were as follows: RCTs on patients with gallstones needing laparoscopic cholecystectomy; induction time administration of intravenous antibiotics as prophylactic dose to prevent SSI; and had at least one outcomes of interest as described above. The studies were included regardless of sample size, origin of study, age of the participant, gender of the participant and the language in which the study was published.
Interventions
The administration of single dose of intravenous antibiotics as prophylactic measure to prevent SSI.
Outcome of interest
We evaluated the length of stay in hospital, all infective complications, superficial SSI, deep SSI, distant infections and deep space infection. These outcomes were defined according to the original studies.
Risk of bias assessment
The methodological quality of the included studies was assessed by MSS and SR as recommended by the Cochrane Collaboration using the “Risk of Bias Assessment Tool”. This included random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, and selective outcome reporting. Disagreement was resolved by a third reviewer (KKS). The critical appraisal tool to score the quality of included trials was also adopted from the published guidelines of Jadad et al. (11) and Chalmers et al. (12). The short summary of the resulting evidence was presented in a tabulated form by using tool GradePro® (13), provided by the Cochrane Collaboration.
Statistical analysis
The efficacy of single dose of intravenous antibiotics was directly compared and pooled for each outcome of interest if there were at least two studies for each comparison. The odds ratio (OR) and standardized mean difference (SMD) were estimated and pooled across studies using a random-effect model. Heterogeneity was assessed using Cochrane Q test and I2 statistic. The statistical analysis of the data was conducted according to the guidelines provided by the Cochrane Collaboration including the use of RevMan 5.3® statistical software, and the use of forest plots for the graphical display of the combined outcomes (14-19).
Results
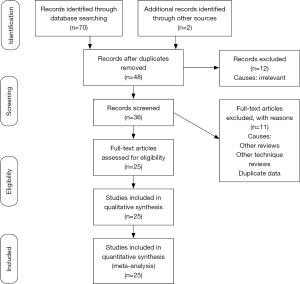
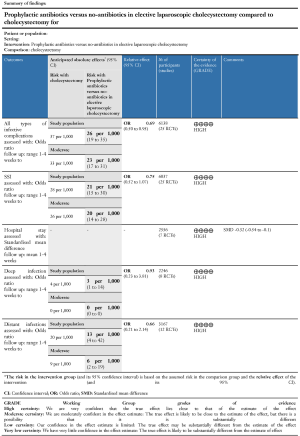
The PRISMA flowchart regarding literature search outcome and study screening pattern is explained in Figure 1. Twenty-five randomized, controlled trials (20-44) on 6,138 patients compared the use of prophylactic induction-time antibiotics. There were 3,099 patients recruited in antibiotics group and 3,039 patients were in no-antibiotics group. The quality of included randomized, controlled trials was moderate to high on Jadad & Chalmers scoring system owing to the utilization of computer generated randomization technique, optimum implementation of power calculations encompassing issues of type I and type II errors, adequate concealment protocol, blinding and the use of intention-to-treat analysis. The short summary and generated evidence is presented in Figure 2 analysed on GradePro.
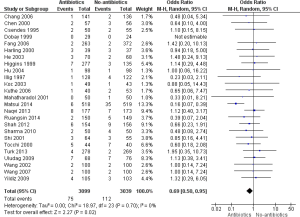
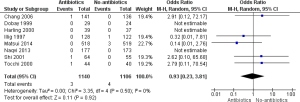
Overall postoperative infective complications
There was no heterogeneity [Tau2 =0.00, chi2 =18.97, df =23, (P=0.70); I2=0%] among included trials. In the random effects model analysis (OR, 0.69; 95% CI, 0.50–0.95; Z=2.27; P=0.02), the risk of developing postoperative infective complications was statistically lower in patients receiving prophylactic antibiotics prior to undergoing ELC (Figure 3).
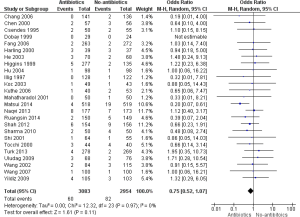
Superficial and deep wound SSI
There was no heterogeneity [Tau2 =0.00, chi2 =12.32, df =23, (P=0.97); I2=0%] among included trials. In the random effects model analysis (OR, 0.75; 95% CI, 0.52–1.07; Z=1.61; P=0.11), the risk of developing superficial and deep wound SSI was lower in antibiotics group but it could not reach the statistical significance (Figure 4).
Deep space SSI
There was no heterogeneity [Tau2 =0.00, chi2 =3.35, df =4, (P=0.50); I2=0%] among included trials. In the random effects model analysis (OR, 0.93; 95% CI, 0.23–3.81; Z=0.11; P=0.92), the risk of developing superficial and deep wound SSI were similar in both groups (Figure 5).
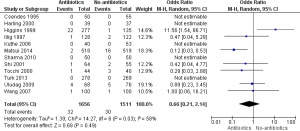
Distant infections
There was moderate heterogeneity [Tau2 =1.39, chi2 =14.27, df =6, (P=0.03); I2=58%] among included trials. In the random effects model analysis (OR, 0.66; 95% CI, 0.21–2.14; Z=0.68; P=0.49), the risk of developing distant infections was lower in antibiotics group but it could not reach the statistical significance (Figure 6).
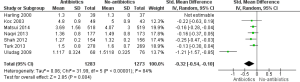
Duration of hospital stay
There was significant heterogeneity [Tau2 =0.06, chi2 =31.99, df =5, (P<0.00001); I2=84%] among included trials. In the random effects model (OR, −0.32; 95% CI, −0.54–−0.10; Z=2.85; P=0.004), the duration of hospital stay was statistically shorter in patients who received prophylactic antibiotics (Figure 7).
Discussion
Summary of main results
Based upon the findings of current study of 25 RCTs on 6,138 patients evaluating the infective complications in patients undergoing ELC, the risk of SSI, distant infection and residual abscess was lower in the antibiotics group but statistical significance was not reached. However, the risk of overall all type of infective complications was statistically lower in the antibiotics group reflecting the reduced length of hospitalization in the antibiotics group. This study is the first ever review reporting the advantages of using prophylactic antibiotics in patients undergoing ELC to prevent infective complications of all types instead of looking at SSI only.
Overall completeness and applicability of evidence
The resulting evidence presented in this article is pertinent to patients undergoing ELC only does not investigate the extended role of prophylactic antibiotics in patients with hot gallbladder. Despite the reporting of several systematic reviews and meta-analyses (7-10) reporting and arguing the non-beneficial role of prophylactic antibiotics for a decade or so, only current study provide evidence on the beneficial role of prophylactic antibiotics and it may be acceptable to recommend the routine use of antibiotics at induction time in patients undergoing ELC.
Quality of evidence
This study reports a total of 6,138 participants from 25 randomized, controlled trials undergoing ELC reporting post-operative infective complications of all types as primary outcome preferentially to highlight the beneficial or non-beneficial role prophylactic antibiotics. The risk of bias in the included trials was very low when scored against the standard quality guidelines and therefore, the quality of resulting evidence may be considered adequate (Figure 2). The bile spillage rate and the need of antibiotics on “as required” bases were inadequately reported in the included trials and therefore, an isolated sub-group analysis of these patients was not possible. This phenomenon may have influenced the final outcome of infective complications. Other confounding factors which might have influenced the final outcome of the postoperative infective complications include the use of variable number and size of ports for ELC; type, duration and dosage of antibiotics; use of extraction endo-bag at surgeons’ discretion; and use of placebo versus no-placebo in non-antibiotics group.
Potential biases in the review process
Authors implemented the standard Cochrane Collaboration methodology to perform the statistical analysis, interpretation as well as to present the quality of evidence. The low risk of bias was mainly attributable to the presence of blinding and allocation concealment in the majority of the studies. Presence of adequate randomization technique and optimum utilization of the power calculations in all included trials provided adequate strength to generate higher level of evidence. The bile spillage rate and the need of antibiotics on “as required” bases were inadequately reported in the included trials and therefore, an isolated sub-group analysis of these patients was not possible. This phenomenon may have influenced the final outcome of infective complications. Other confounding factors which might have influenced the final outcome of the postoperative infective complications include the use of variable number and size of ports for ELC; type, duration and dosage of antibiotics; use of extraction endo-bag at surgeons’ discretion; and use of placebo versus no-placebo in non-antibiotics group.
Agreement and disagreement with other published evidence
The findings of current meta-analysis are not in accordance with the conclusions of the previously published reviews (7-10) which demonstrated that the use of prophylactic antibiotics in patients undergoing ELC did not reduce SSI rate. However, this study provides up to date, comprehensive and cumulative evidence favouring the use of prophylactic antibiotics on these patients to reduce overall post-operative infective complications rather focusing on SSIs only.
Implications for practice and future research
This study quite successfully validate that the prophylactic use of antibiotics is effective in reducing the post-operative infective complications in patients undergoing ELC. However, the aforementioned confounding factors potentially influencing the final outcomes must be acknowledged and attempts must be made to generate less biased evidence by removing these limitations. These results cannot be generalized in all patients undergoing ELC because the prophylactic strategy for post-operative infective complications is multi-dimensional which also include pre-operative and per-operative measures for optimum reduction. Evaluation of infective complications in group of patients with perforated gallbladder during ELC needs another randomized, trial comparing with non-perforated gallbladder to find the necessity and duration of antibiotics prophylaxis. In addition, trials targeting type and duration of antibiotics prophylaxis are also required to avoid study sample contamination by modifiable confounding factors.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Henry ML, Carey LC. Complications of cholecystectomy. Surg Clin North Am 1983;63:1191-204. [Crossref] [PubMed]
- Urban JA. Cost analysis of surgical site infections. Surg Infect (Larchmt) 2006;7 Suppl 1:S19-22. [Crossref] [PubMed]
- Fry DE. The economic of costs of surgical site infections. Surg Infect (Larchmt) 2002;3 Suppl 1:S37-43. [Crossref] [PubMed]
- Cranny G, Elliott R, Weatherly H, et al. A systematic review and economic model of switching from non-glycopeptide to glycopeptide antibiotic prophylaxis for surgery. Health Technol Assess 2008;12: iii-iv, xi-xii, 1-147.
- Broex EC, van Asselt AD, Bruggeman CA, van Tiel FH. Surgical site infections. How high are the cost? J Hosp Infect 2009;72:193-201. [Crossref] [PubMed]
- Barnes CL. Overview: the health care burden and financial costs of surgical site infections. Am J Orthop (Belle Mead NJ) 2011;40:2-5. [PubMed]
- Choudhary A, Bechtold ML, Puli SR, et al. Role of prophylactic antibiotics in laparoscopic cholecystectomy: a meta-analysis. J Gastrointest Surg 2008;12:1847-53. [Crossref] [PubMed]
- Sanabria A, Dominguez LC, Valdivieso E, et al. Antibiotic prophylaxis for patients undergoing elective laparoscopic cholecystectomy. Cochrane Database Syst Rev 2010;8:CD005265. [PubMed]
- Al-Ghnaniem R, Benjamin IS, Patel AG. Meta-analysis suggests antibiotic prophylaxis is not warranted in low-risk patients undergoing laparoscopic cholecystectomy. Br J Surg 2003;90:365-6. [Crossref] [PubMed]
- Catarci M, Mancini S, Gentileschi P, et al. Antibiotic prophylaxis in elective laparoscopic cholecystectomy. Lack of need or lack of evidence? Surg Endosc 2004;18:638-41. [Crossref] [PubMed]
- Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996;17:1-12. [Crossref] [PubMed]
- Chalmers TC, Smith H Jr, Blackburn B, et al. A method for assessing the quality of a randomized control trial. Control Clin Trials 1981;2:31-49. [Crossref] [PubMed]
- Cochrane IMS. Available online: [accessed on 10/03/2018].http://ims.cochrane.org/revman/otherresources/gradepro/download
- Higgins JPT, Green S (eds). Cochrane Handbook for Systematic Reviews of Interventions Version 5·0·0 (updated February 2008). Available online: [accessed on 10/07/2016].http://www.cochrane-handbook.org
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan 5.3) [Computer program]. Copenhagen; 2012. Available online: [accessed on 25/04/22018].http://nordic.cochrane.org
- Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [Crossref] [PubMed]
- DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177-88. [Crossref] [PubMed]
- Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539-58. [Crossref] [PubMed]
- Egger M, Smith GD, Altman DG. editors. Systematic reviews in healthcare. London: BMJ Publishing, 2006.
- Chang WT, Lee KT, Shih-Chang Chuang SC, et al. The impact of prophylactic antibiotics on postoperative infection complication in elective laparoscopic cholecystectomy: a prospective randomized study. Am J Surg 2006;191:721-5. [Crossref] [PubMed]
- Chen WJ, Mou YP, Li JD. Use of Antibiotic Prophylaxis in Elective Laparoscopic Cholecystectomies. Zhejiang Medical Journal 2000;22:684-5.
- Csendes A, Silva A, Burdiles P, et al. Antibiotic Prophylaxis in Laparoscopic Cholecystectomies: Prospective Randomised Trial. Revista Chilena de Cirugia 1995;47:145-7.
- Dobay KJ, Freier DT, Albear P, et al. The absent role of prophylactic antibiotics in low-risk patients undergoing laparoscopic cholecystectomy. Am Surg 1999;65:226-8. [PubMed]
- Fang ZH, Hou YF, Wu W. The value of using antibiotics in perioperative period of laparoscopic cholecystectomy. Journal of Laparoscopic Surgery 2006;11:250-1.
- Harling R, Moorjani N, Perry C, et al. A prospective, randomised trial of prophylactic antibiotics versus bag extraction in the prophylaxis of wound infection in laparoscopic cholecystectomy. Ann R Coll Surg Engl 2000;82:408-10. [PubMed]
- He Y, Jin X. Zhang X. A prospective trial of perioperative antibiotic prophylaxis for prevention of post operative infection in patients undergoing laparoscopic cholecystectomy. Clinical Medicine 2003;23:4-5.
- Higgins A, London J, Charland S, et al. Prophylactic antibiotics for elective laparoscopic cholecystectomyare they necessary? JAMA Surgery 1999;134:6-10.
- Hu M, Chen B, Song X. Preoperative antibiotic prophylaxis in elective laparoscopic cholecystectomy: a prospective trial. Chinese Journal of General Surgery 2004;19:639-40.
- Illig KA, Schmit E, Cavanaugh J, et al. Are prophylactic antibiotics required for elective laparoscopic cholecystectomy? J Am Coll Surg 1997;184:353-6. [PubMed]
- Koc M, Zulifikaroglu B, Kece C. A prospective randomised study of prophylactic antibiotics in elective cholecystectomy Surg Endosc 2003;17:1716-8. [Crossref] [PubMed]
- Kuthe SA, Kaman L, Verma GR, et al. Evaluation of the role of prophylactic antibiotics in elective laparoscopic cholecystectomy: a prospective randomized trial. Trop Gastroenterol 2006;27:54-7. [PubMed]
- Mahatharadol V. A revaluation of antibiotic prophylaxis in laparoscopic cholecystectomy: a randomized controlled trial. J Med Assoc Thai 2001;84:105-8. [PubMed]
- Matsui Y, Satoi S, Kaibori M, et al. Antibiotic prophylaxis in laparoscopic cholecystectomy: a randomized controlled trial. PLoS One 2014;9:e106702. [Crossref] [PubMed]
- Naqvi MA, Mehraj A, Ejaz R, et al. Role of prophylactic antibiotics in low risk elective laparoscopic cholecystectomy: is there a need? J Ayub Med Coll Abbottabad 2013;25:172-4. [PubMed]
- Ruangsin S, Laohawiriyakamol S, Sunpaweravong S, et al. The efficacy of cefazolin in reducing surgical site infection in laparoscopic cholecystectomy: a prospective randomized double-blind controlled trial Surg Endosc 2015;29:874-81. [Crossref] [PubMed]
- Shah JN, Maharjan SB, Paudyal S. Routine use of antibiotic prophylaxis in low-risk laparoscopic cholecystectomy is unnecessary: A randomized clinical trial Asian J Surg 2012;35:136-9. [Crossref] [PubMed]
- Sharma N, Kumar Garg P, Hadke NS, et al. Role of prophlactic antibiotics in laparoscopic cholecystectomy and risk factors for surgical site infection: A randomized controlled trial. Surg Infect (Larchmt) 2010;11:367-70. [Crossref] [PubMed]
- Shi HX, Zhang XD, Sun T. Evaluation of the use of antibiotic prophylaxis in elective laparoscopic cholecystectomy. J Surg Conc Prac 2001;6:403-4.
- Tocchi A, Lepre L, Costa G, et al. The Need for antibiotic prophylaxis in elective laparoscopic cholecystectomy: A prospective randomized study. Arch Surg 2000;135:67-70. [Crossref] [PubMed]
- Turk E, Karaguelle E, Serefhanoglu K, et al. Effect of cefazolin prophylaxis on postoperative infectious complications in elective laparoscopic cholecystectomy: A prospective randomized study. Iran Red Crescent Med J 2013;15:581-6. [Crossref] [PubMed]
- Uludag M, Yetkin G, Citgez B. The role of prophylactic antibiotics in elective laparoscopic cholecystectomy. JSLS 2009;13:337-41. [PubMed]
- Wang LB, Chen WJ, Song XY, et al. Antibiotic prophylaxis in elective laparoscopic cholecystectomy: a prospective trial. Chinese Journal of Nosocomiology 2002;12:845-6.
- Wang B, Shen LG, Li LB. Necessity of prophylactic antibiotics use in patients undergoing elective laparoscopic cholecystectomy. Clinical Education of General Practice 2007;5:124-5.
- Yildiz B, Abbasoglu O, Tirnaksiz B, et al. Determinants of postoperative infection after laparoscopic cholecystectomy. Hepatogastroenterology 2009;56:589-92. [PubMed]
Cite this article as: Sajid MS, Bovis J, Rehman S, Singh KK. Prophylactic antibiotics at the time of elective cholecystectomy are effective in reducing the post-operative infective complications: a systematic review and meta-analysis. Transl Gastroenterol Hepatol 2018;3:22.