Hepatocellular cancer and recurrence after liver transplantation: what about the impact of immunosuppression?
Introduction
In 1963 medicine and surgery have been revolutionized by the introduction in clinical practice of liver transplantation (LT) (1). After a difficult, 20-year long, period of “trial and error”, two major events made its breakthrough happen. The first one was the introduction of a selective immunosuppressant, the cyclosporine A (CyA), a calcineurin inhibitor (CNI); the second one the “1983 National Institutes of Health Consensus Conference”, which valued LT as “a promising alternative to current therapy in the management of the late phase of several forms of serious—benign and malignant—liver disease”. This conclusion was based on the, at that time existing, worldwide experience comprising only 540 transplants done in four medical centres, Denver, Cambridge, Groningen and Hannover during the period 1963–1983 (2). Since then the LT experience literally exploded. So far more than 300,000 procedures have been performed.
The cumulated experience, gathered during half a century, enabled to answer almost all the questions related to benign end-stage liver and liver-based metabolic diseases. Conversely, the transplant community still struggles with many answers to medical and, even more so, ethical questions related to the best treatment of primary malignant liver diseases, around 90% of them consisting of HCC.
Innumerable studies have been and are being conducted in order to improve selection/inclusion criteria for LT as well as liver allocation algorithms in order to balance principles of utility (or good outcome without recurrence) and justice (or good access without interference with the “transplant chance” of patients with benign liver diseases) in the ever increasing population of HCC patients. Almost all studies focused initially on morphologic and, more recently, biologic tumour characteristics. The combination of several features made it possible to build different scores, criteria… and opinions! Today different organ allocation organisms handle somewhat different scores all aiming to distribute in the best possible way scarce liver allografts to the individual HCC patient looking thereby in particular at disease-free survival (DFS) (3-7). It is curious that one of the most important confounders related to DFS of whatever oncologic treatment, notably, the immunosuppressive state, and thus the use of IS, has been sparsely addressed in this context. Logically one should seek for a balance between immunologic (graft rejection) and oncologic risk (development of tumour recurrence and/or also de novo tumour formation) in order to boost outcomes in HCC liver recipients. Yet much confusion persists as exemplified by one of “2010 Zurich Consensus Conference on HCC and LT” recommendations: “there is currently insufficient evidence from clinical trials to base a recommendation for choosing the type or dose of IS therapy to influence the incidence of HCC recurrence or its prognosis” (8). So the debate about the optimal IS after LT in HCC patients is still open.
This article aims to review the available literature concerning the relationship between IS and outcomes of HCC after LT. In view of a deeper understanding, two short updates are first made about selection criteria of HCC patients for LT and about some basic knowledge about IS and oncogenesis. Based on these data as well as on a large experience in both transplant oncology and immunosuppressive management, some personal recommendations will also be provided.
Hepatocellular cancer (HCC) and LT: selection
The concept of LT was originally developed by T. E. Starzl in Denver in order to treat (unresectable) liver tumours. Indeed eight of the worldwide ten first LT attempts were done because of liver malignancies. The 10th patient was the first long-term liver recipient. She died due to tumour recurrence 400 days after LT (9). Five patients presented a HCC, one a cholangiocellular cancer and two colorectal liver metastases. All these indications are today hot topics in almost every hepatology or transplantation meeting.
The idea of total hepatectomy as “the” treatment of liver cancer was further explored during the “adolescent phase” of LT (covering the period 1963–1983). The late R. Pichlmayr greatly fostered the upcoming field of “transplant oncology” (10). However, the enthusiasm of the pioneering centres rapidly declined due to poor long-term outcomes and very high recurrence rates, all explained by the lack of adequate selection criteria. Progressive improvements in surgical technique, postoperative care and selection reversed the tide. The 5-years overall survival (OS) rates improved over the last decades from the low 12% before 1985 to the high 70% long-term survival during the last decade (ELTR data). The major determinant for this success was the introduction of selection criteria, which led to move away from “transplantation of the unresectable HCC” towards “transplantation of the resectable HCC”. The introduction of the Milan Criteria (MC) in 1996 best translated this shift. These are static and morphologic criteria based on both tumour number (up to 3) and diameter (up to 5 cm). Adoption of these inclusion criteria resulted in up to 96% 5 and 10 years DFS, results to be considered as one of the best in the whole field of oncology (11). Therefore, these criteria were rapidly (in total or in part) integrated in almost all algorithms for liver allocation. However, recent experiences questioned the adherence to the restrictive MC as this attitude may unjustifiably exclude at least 20% (and some Eastern experiences even raise this proportion to 60%) of HCC patients from a potentially curative treatment (6,12). In contrast, several papers convincingly showed that the MC can be widened by complementing “static and morphologic” tumour criteria with “dynamic and biologic” ones. Tumour-released molecules, such as α-fetoprotein (AFP) and des-γ-carboxyprothrombin (DCP), also known as protein induced by vitamin K absence-II (PIVKA-II), and inflammatory markers, such as neutrophil-to-lymphocyte ratio (NLR) or platelet-to-lymphocyte ratio (PLR), as well as tumour response to neo-adjuvant locoregional treatments, such as transarterial chemo/radio-embolization and radiofrequency or alcohol ablation, are all independent predictors of dropout before and tumour recurrence after LT (13-18). This “dynamic” approach proved to be valuable enabling to transplant more patients without compromising their outcomes (4-6,18,19).
Combination of both “morphologic and static” and “biologic and dynamic” tumour features has been warmly welcomed in Asian countries due to the explosive development of living donor liver transplantation (LDLT). The LDLT constellation has the major advantage of transforming LT for cancer into an elective, scheduled procedure. Accordingly both “factor tumour” and “factor time” can be controlled and both neo-adjuvant and radical treatment can be intertwined. This opportunity pushed some centres to (re)consider LT in patients presenting macrovascular tumour invasion (20).
The aforementioned static and dynamic tumour characteristics are linked to tumour differentiation, inflammation, molecular features and vascular invasion (21-23).
Immunosuppression (IS) and carcinogenesis
The integrity of the immune system is the mainstay in cancer and infection control. When analysing the 21st-century literature in relation to the incidence of tumour recurrence after LT, the lack of attention paid to the impact of IS on the outcome of liver cancer recipients is surprising. The link between IS and oncogenesis has been unequivocally proven both in laboratory and clinical settings (24-30). The increase in cancer risk has already been ascertained in patients receiving IS as well as in patients with an end-stage organ failure. Nevertheless, only virus-related cancers have a higher incidence after post-transplant IS. Oncogenic viruses can immortalise infected cells by disrupting the cell-cycle control and, in a setting of induced lowered immune surveillance, this phenomenon is likely to cause tumorigenesis (29,30). Basic research is important for further progress in transplantation oncology as demonstrated by the following two examples. Yokoyama showed in 1991 that IS drugs stimulate cancer cell growth (24). In contrast, Guba showed that mammalian target of rapamycin inhibitors (mTORis), including sirolimus or rapamycine (SRL) and everolimus (EVL), interfere with carcinogenesis by inhibiting the PI3K/Akt/mTOR pathway, the key regulator of cellular proliferation and angiogenesis (27). In vivo, the use of mTORis proved to reduce the risk of post-transplant de novo cancers, in particular of non-melanoma skin cancers, in kidney transplanted populations (31,32).
Around 1850 Virchow identified first the relationship between inflammation and cancer. Unravelling this relationship during the 21st century fostered a deeper insight in the process of carcinogenesis (33). Inflammatory parameters such as C-reactive protein, erythrocyte sedimentation rate, NLR, PLR and inflammatory cytokines (such as IL1b, 6, 7 and 17) have all been linked to tumour aggressiveness and recurrence after LT because of their role in promotion of neoangiogenesis and tumour growth. Similarly studies on the type of lymphocytic infiltration in tumour and peritumoral liver tissues also showed that a reduced immune status, as expressed by a disturbed balance between T-regulatory and CD8 lymphocytes, favours tumour aggressiveness and recurrence after transplantation. In summary, tumour-induced inflammation and reduced immune defence against cancer are responsible for increased recurrence (34).
Basic science findings together with many (observational) clinical experiences indicate that not only the type of immunosuppressive drug(s) or scheme(s) but, even more decisively, the total immunosuppressive load plays a role in cancer recurrence. This interaction will gain an ever growing relevance because inclusion criteria for LT are wider and wider and (re-)implementing LT as a treatment for secondary neuro-endocrine and colorectal liver tumours is around the corner.
Beside the issue of HCC recurrence, long-term results in all fields of organ transplantation are seriously compromised not only by the occurrence of cardiovascular and metabolic (in 30% to 40% of recipients), renal (18% of recipients) and infectious complications but also by de novo tumour formation (more than 10% of recipients). These are the major causes of patient loss in presence of a functioning graft (35,36).
HCC, LT and IS
Despite compelling data, very few studies have addressed the impact of IS on outcomes in HCC recipients and, when done, they lack high level of evidence due to the heterogeneity of the studied patient cohorts and the lack of prospective design and randomization (37,38). Moreover, this key field of transplant oncology surely suffered from the tsunami of industry-driven IS trials in which “minimization” approach is not addressed at all or limited to the dose reduction or (timely) elimination of one specific drug in favour of another one. The best example of such design is the recent study centred on the T-cell co-stimulation blocker belatacept, examining the benefit of a quadruple IS scheme in LT (39).
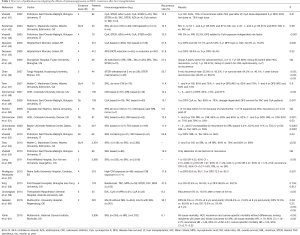
Till 2016 we found in the literature 21 articles dealing with LT and IS, of which only one is prospective and randomized and two are SRL-related meta-analyses (Table 1) (37). Six ones studied the impact of CNI use or load, eleven the impact of SRL, two the steroid use or withdrawal and one the impact of ATG/OKT3 and steroid-based IS. Overall recurrence rate ranged from 12% to 54%.
Full table
From these observational studies and two meta-analyses including 474 and 2,950 HCC recipients experiences two conclusions can be drawn: (I) the higher the exposure to CNIs, either CyA or tacrolimus (TAC), the higher is the recurrence risk and (II) mTOR inhibitors reduce the recurrence risk (49,56,57,62).
The Rodríguez-Perálvarez’ retrospective minimization study offers strong evidence for a significantly lower recurrence rate (14.7% vs. 27.7%) in case of low CNI exposure during the first post-LT month (57).
Unfortunately the protective effect of mTORi has been seriously weakened by the results of the, so far only, large, transcontinental, multicentre, prospective, randomized SILVER study (60). This trial was based on SRL and merely showed a lower recurrence rate in early HCC at 3 years. This effect was erased at 5 years. Two major remarks must be made in relation to these findings. First the results obtained in T2 HCC lesions (this means MC-in lesions) at 3 years are inferior to those obtained in most transplant centres in the absence of mTORi-based IS (11,63). Second the results of this large patients’ cohort suffer from high heterogeneity: the only constant IS factor was the addition of SRL to very different IS schemes. Each centre had his own “IS cocktail” with or without steroids, with or without steroid withdrawal, early or late introduction of CNI, presence or absence of induction therapies, using different kinds of anti-lymphocytic sera or antibodies.
The role of mycophenolic acid (MPA), an antimetabolite, is contradictory but its impact in vivo seems negligible (64-66). The use of azathioprine (AZA), another antimetabolite known to induce non-skin malignancy in LT, has not been analysed in respect of HCC recurrence (67). The same can be stated for the use of corticosteroids, anti-lymphocytic sera and anti-interleukin-2 receptor α antibodies (46,58,68-73).
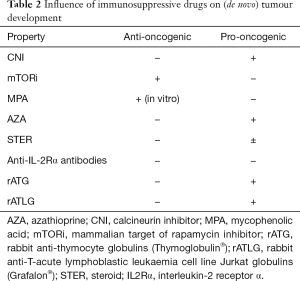
Few solid conclusions can be made from this literature review about the true impact of any specific immunosuppressant on the real incidence of HCC recurrence. Nevertheless, IS load seems to play a determinant role in cancer recurrence (49,57). Basic clinical research and many observational studies favour this hypothesis. The most relevant data about the several categories of IS drugs in relation to the risk of malignancy are listed in Table 2 (34). The minimization approach is of special value in an era where transplant oncology is slowly but steadily becoming the first indication in adult LT. More and more patients are undergoing transplantation with MC-out or advanced HCC based on the “modern” oncologic selection process, which integrates both tumour morphology and biology (18,19,74,75). Moreover, minimization strategies are justified by the intrinsic immunosuppressed status oncologic patients usually display and by the immunologic privilege of the liver, which allows a substantial reduction in IS load without compromising both patient and graft survival (38,76,77). Further broadening of indications for LT in case of primary and secondary liver tumours will forcibly require adjuvant chemotherapy (78), a reason more to opt for immunosuppressive minimization protocols.
Full table
Conclusions
Today we are on the brink of a real (r)evolution both in LT and oncology. The more widespread use of machine perfusion for severely compromised deceased-donor livers (79) and of living-donor LT, together with the possible eradication of viral diseases, will lead to an ever growing number of transplants for not only primary but also secondary liver tumours.
Sound oncologic principles from all other fields taught us that outcomes optimization entails a combination of tumour biology criteria, neo- and adjuvant (even including systemic chemotherapy) treatments and, last but not least, adapted, minimized and individualized IS. In the absence of well-designed studies, no firm conclusions can be drawn about the impact of a given immunosuppressive drug on recurrence or de novo development of malignancies. In order to significantly influence HCC recurrence after LT it will be necessary to reduce as much as possible the immunosuppressive load. mTOR inhibitors may possibly play a favourable role in this context, especially in case of advanced tumour burden. The advent of immunotherapy will be an additional tool in the race against liver cancer (80).
The final step in the optimization of patients’ selection for a (potential curative) transplant procedure will be the integration of the “static-to-dynamic” paradigm switch into the intention-to-treat benefit concept, which looks at the difference between pre- and post-transplant outcomes (81). Outweighing transplant utility (post-LT outcome read recurrence) and urgency (pre-LT outcome) will be the best guarantee to assure a transplant to the highest possible number of patients with the best results. Adapted immunosuppressive therapy will be an important player in this scenario.
Acknowledgements
This work was supported by Hepatotransplant and Euroliver Foundation.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Starzl TE, Marchioro TL, Vonkaulla KN, et al. Homotransplantation of the liver in humans. Surg Gynecol Obstet 1963;117:659-76. [PubMed]
- Van Thiel DH, Schade RR, Starzl TE. After 20 years, liver transplantation comes of age. Ann Intern Med 1983;99:854-6. [Crossref] [PubMed]
- Francoz C, Belghiti J, Castaing D, et al. Model for end-stage liver disease exceptions in the context of the French model for end-stage liver disease score-based liver allocation system. Liver Transpl 2011;17:1137-51. [Crossref] [PubMed]
- Takada Y, Tohyama T, Watanabe J. Biological markers of hepatocellular carcinoma for use as selection criteria in liver transplantation. J Hepatobiliary Pancreat Sci 2015;22:279-86. [Crossref] [PubMed]
- Sugawara Y, Tamura S, Makuuchi M. Living donor liver transplantation for hepatocellular carcinoma: Tokyo University series. Dig Dis 2007;25:310-2. [Crossref] [PubMed]
- Xia W, Ke Q, Guo H, et al. Expansion of the Milan criteria without any sacrifice: combination of the Hangzhou criteria with the pre-transplant platelet-to-lymphocyte ratio. BMC Cancer 2017;17:14. [Crossref] [PubMed]
- Mehta N, Yao FY. Hepatocellular cancer as indication for liver transplantation: pushing beyond Milan. Curr Opin Organ Transplant 2016;21:91-8. [Crossref] [PubMed]
- Clavien PA, Lesurtel M, Bossuyt PM, et al. Recommendations for liver transplantation for hepatocellular carcinoma: an international consensus conference report. Lancet Oncol 2012;13:e11-22. [Crossref] [PubMed]
- Starzl TE, Groth CG, Brettschneider L, et al. Orthotopic homotransplantation of the human liver. Ann Surg 1968;168:392-415. [Crossref] [PubMed]
- Pichlmayr R, Weimann A, Oldhafer KJ, et al. Appraisal of transplantation for malignant tumours of the liver with special reference to early stage hepatocellular carcinoma. Eur J Surg Oncol 1998;24:60-7. [Crossref] [PubMed]
- Mazzaferro V, Regalia E, Doci R, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med 1996;334:693-9. [Crossref] [PubMed]
- Toso C, Meeberg G, Hernandez-Alejandro R, et al. Total tumor volume and alpha-fetoprotein for selection of transplant candidates with hepatocellular carcinoma: A prospective validation. Hepatology 2015;62:158-65. [Crossref] [PubMed]
- Allard MA, Sebagh M, Ruiz A, et al. Does pathological response after transarterial chemoembolization for hepatocellular carcinoma in cirrhotic patients with cirrhosis predict outcome after liver resection or transplantation? J Hepatol 2015;63:83-92. [Crossref] [PubMed]
- Lai Q, Avolio AW, Graziadei I, et al. Alpha-fetoprotein and modified response evaluation criteria in solid tumors progression after locoregional therapy as predictors of hepatocellular cancer recurrence and death after transplantation. Liver Transpl 2013;19:1108-18. [PubMed]
- Mehta N, Heimbach J, Harnois DM, et al. Validation of a Risk Estimation of Tumor Recurrence After Transplant (RETREAT) Score for Hepatocellular Carcinoma Recurrence After Liver Transplant. JAMA Oncol 2017;3:493-500. [Crossref] [PubMed]
- Otto G, Schuchmann M, Hoppe-Lotichius M, et al. How to decide about liver transplantation in patients with hepatocellular carcinoma: size and number of lesions or response to TACE? J Hepatol 2013;59:279-84. [Crossref] [PubMed]
- Duvoux C, Roudot-Thoraval F, Decaens T, et al. Liver transplantation for hepatocellular carcinoma: a model including alpha-fetoprotein improves the performance of Milan criteria. Gastroenterology 2012;143:986-94 e3; quiz e14-5.
- Lai Q, Nicolini D, Inostroza Nunez M, et al. A novel prognostic index in patients with hepatocellular cancer waiting for liver transplantation: time-radiological-response-alpha-fetoprotein-inflammation (TRAIN) score. Ann Surg 2016;264:787-96. [Crossref] [PubMed]
- Hong SK, Lee KW, Kim HS, et al. Living donor liver transplantation for hepatocellular carcinoma in Seoul National University. Hepatobiliary Surg Nutr 2016;5:453-60. [Crossref] [PubMed]
- Lee KW, Suh SW, Choi Y, et al. Macrovascular invasion is not an absolute contraindication for living donor liver transplantation. Liver Transpl 2017;23:19-27. [Crossref] [PubMed]
- Sapisochin G, Goldaracena N, Laurence JM, et al. The extended Toronto criteria for liver transplantation in patients with hepatocellular carcinoma: A prospective validation study. Hepatology 2016;64:2077-88. [Crossref] [PubMed]
- Lai Q, Lerut JP. Hepatocellular cancer: how to expand safely inclusion criteria for liver transplantation. Curr Opin Organ Transplant 2014;19:229-34. [Crossref] [PubMed]
- Mínguez B, Hoshida Y, Villanueva A, et al. Gene-expression signature of vascular invasion in hepatocellular carcinoma. J Hepatol 2011;55:1325-31. [Crossref] [PubMed]
- Yokoyama I, Carr B, Saitsu H, et al. Accelerated growth rates of recurrent hepatocellular carcinoma after liver transplantation. Cancer 1991;68:2095-100. [Crossref] [PubMed]
- Shinozuka H, Warty VS, Masuhara M, et al. Effect of FK 506 on experimental liver carcinogenesis. Transplant Proc 1991;23:3197-9. [PubMed]
- Wimmer CD, Angele MK, Schwarz B, et al. Impact of cyclosporine versus tacrolimus on the incidence of de novo malignancy following liver transplantation: a single center experience with 609 patients. Transpl Int 2013;26:999-1006. [Crossref] [PubMed]
- Andrassy J, Graeb C, Rentsch M, et al. mTOR inhibition and its effect on cancer in transplantation. Transplantation 2005;80:S171-4. [Crossref] [PubMed]
- Hojo M, Morimoto T, Maluccio M, et al. Cyclosporine induces cancer progression by a cell-autonomous mechanism. Nature 1999;397:530-4. [Crossref] [PubMed]
- Piselli P, Busnach G, Fratino L, et al. De novo malignancies after organ transplantation: focus on viral infections. Curr Mol Med 2013;13:1217-27. [Crossref] [PubMed]
- Mazzucotelli V, Piselli P, Verdirosi D, et al. De novo cancer in patients on dialysis and after renal transplantation: North-western Italy, 1997-2012. J Nephrol 2017. [Epub ahead of print]. [Crossref] [PubMed]
- Piselli P, Serraino D, Segoloni GP, et al. Risk of de novo cancers after transplantation: results from a cohort of 7217 kidney transplant recipients, Italy 1997-2009. Eur J Cancer 2013;49:336-44. [Crossref] [PubMed]
- Opelz G, Unterrainer C, Susal C, et al. Immunosuppression with mammalian target of rapamycin inhibitor and incidence of post-transplant cancer in kidney transplant recipients. Nephrol Dial Transplant 2016;31:1360-7. [Crossref] [PubMed]
- Balkwill F, Mantovani A. Cancer and inflammation: implications for pharmacology and therapeutics. Clin Pharmacol Ther 2010;87:401-6. [Crossref] [PubMed]
- Cescon M, Bertuzzo VR, Ercolani G, et al. Liver transplantation for hepatocellular carcinoma: role of inflammatory and immunological state on recurrence and prognosis. World J Gastroenterol 2013;19:9174-82. [Crossref] [PubMed]
- Neuberger JM, Bechstein WO, Kuypers DR, et al. Practical recommendations for long-term management of modifiable risks in kidney and liver transplant recipients: a guidance report and clinical checklist by the consensus on managing modifiable risk in transplantation (COMMIT) group. Transplantation 2017;101:S1-S56. [Crossref] [PubMed]
- Rao KV, Kasiske BL, Dahl DC, et al. Long-term results and complications of renal transplantation: the Hennepin experience. Clin Transpl 1997.119-24. [PubMed]
- Schnitzbauer AA, Schlitt HJ, Geissler EK. Influence of immunosuppressive drugs on the recurrence of hepatocellular carcinoma after liver transplantation: a gap between basic science and clinical evidence. Transplantation 2011;91:1173-6. [Crossref] [PubMed]
- Rodríguez-Perálvarez M, De la Mata M, Burroughs AK. Liver transplantation: immunosuppression and oncology. Curr Opin Organ Transplant 2014;19:253-60. [Crossref] [PubMed]
- Klintmalm GB, Feng S, Lake JR, et al. Belatacept-based immunosuppression in de novo liver transplant recipients: 1-year experience from a phase II randomized study. Am J Transplant 2014;14:1817-27. [Crossref] [PubMed]
- Howick J, Chalmers I, Glasziou P, et al. Explanation of the 2011 oxford centre for evidence-based medicine (OCEBM) levels of evidence (background document). Oxford Centre for Evidence-Based Medicine. Available online: http://www.cebm.net/ocebm-levels-of-evidence/
- Vivarelli M, Bellusci R, Cucchetti A, et al. Low recurrence rate of hepatocellular carcinoma after liver transplantation: better patient selection or lower immunosuppression? Transplantation 2002;74:1746-51. [Crossref] [PubMed]
- Kneteman NM, Oberholzer J, Al Saghier M, et al. Sirolimus-based immunosuppression for liver transplantation in the presence of extended criteria for hepatocellular carcinoma. Liver Transpl 2004;10:1301-11. [Crossref] [PubMed]
- Vivarelli M, Cucchetti A, Piscaglia F, et al. Analysis of risk factors for tumor recurrence after liver transplantation for hepatocellular carcinoma: key role of immunosuppression. Liver Transpl 2005;11:497-503. [Crossref] [PubMed]
- Decaens T, Roudot-Thoraval F, Bresson-Hadni S, et al. Role of immunosuppression and tumor differentiation in predicting recurrence after liver transplantation for hepatocellular carcinoma: a multicenter study of 412 patients. World J Gastroenterol 2006;12:7319-25. [Crossref] [PubMed]
- Zhou J, Fan J, Wang Z, et al. Conversion to sirolimus immunosuppression in liver transplantation recipients with hepatocellular carcinoma: Report of an initial experience. World J Gastroenterol 2006;12:3114-8. [Crossref] [PubMed]
- Chen ZS, He F, Zeng FJ, et al. Early steroid withdrawal after liver transplantation for hepatocellular carcinoma. World J Gastroenterol 2007;13:5273-6. [Crossref] [PubMed]
- Toso C, Meeberg GA, Bigam DL, et al. De novo sirolimus-based immunosuppression after liver transplantation for hepatocellular carcinoma: long-term outcomes and side effects. Transplantation 2007;83:1162-8. [Crossref] [PubMed]
- Zimmerman MA, Trotter JF, Wachs M, et al. Predictors of long-term outcome following liver transplantation for hepatocellular carcinoma: a single-center experience. Transpl Int 2007;20:747-53. [Crossref] [PubMed]
- Vivarelli M, Cucchetti A, La Barba G, et al. Liver transplantation for hepatocellular carcinoma under calcineurin inhibitors: reassessment of risk factors for tumor recurrence. Ann Surg 2008;248:857-62. [Crossref] [PubMed]
- Nocera A, Andorno E, Tagliamacco A, et al. Sirolimus therapy in liver transplant patients: an initial experience at a single center. Transplant Proc 2008;40:1950-2. [Crossref] [PubMed]
- Zimmerman MA, Trotter JF, Wachs M, et al. Sirolimus-based immunosuppression following liver transplantation for hepatocellular carcinoma. Liver Transpl 2008;14:633-8. [Crossref] [PubMed]
- Chinnakotla S, Davis GL, Vasani S, et al. Impact of sirolimus on the recurrence of hepatocellular carcinoma after liver transplantation. Liver Transpl 2009;15:1834-42. [Crossref] [PubMed]
- Vivarelli M, Dazzi A, Zanello M, et al. Effect of different immunosuppressive schedules on recurrence-free survival after liver transplantation for hepatocellular carcinoma. Transplantation 2010;89:227-31. [Crossref] [PubMed]
- Toso C, Merani S, Bigam DL, et al. Sirolimus-based immunosuppression is associated with increased survival after liver transplantation for hepatocellular carcinoma. Hepatology 2010;51:1237-43. [Crossref] [PubMed]
- Vivarelli M, Dazzi A, Cucchetti A, et al. Sirolimus in liver transplant recipients: a large single-center experience. Transplant Proc 2010;42:2579-84. [Crossref] [PubMed]
- Liang W, Wang D, Ling X, et al. Sirolimus-based immunosuppression in liver transplantation for hepatocellular carcinoma: a meta-analysis. Liver Transpl 2012;18:62-9. [Crossref] [PubMed]
- Rodríguez-Perálvarez M, Tsochatzis E, Naveas MC, et al. Reduced exposure to calcineurin inhibitors early after liver transplantation prevents recurrence of hepatocellular carcinoma. J Hepatol 2013;59:1193-9. [Crossref] [PubMed]
- Xing T, Huang L, Yu Z, et al. Comparison of steroid-free immunosuppression and standard immunosuppression for liver transplant patients with hepatocellular carcinoma. PLoS One 2013;8:e71251. [Crossref] [PubMed]
- Cholongitas E, Goulis I, Theocharidou E, et al. Everolimus-based immunosuppression in liver transplant recipients: a single-centre experience. Hepatol Int 2014;8:137-45. [Crossref] [PubMed]
- Geissler EK, Schnitzbauer AA, Zulke C, et al. Sirolimus use in liver transplant recipients with hepatocellular carcinoma: a randomized, multicenter, open-label phase 3 trial. Transplantation 2016;100:116-25. [Crossref] [PubMed]
- Yanik EL, Chinnakotla S, Gustafson SK, et al. Effects of maintenance immunosuppression with sirolimus after liver transplant for hepatocellular carcinoma. Liver Transpl 2016;22:627-34. [Crossref] [PubMed]
- Menon KV, Hakeem AR, Heaton ND. Meta-analysis: recurrence and survival following the use of sirolimus in liver transplantation for hepatocellular carcinoma. Aliment Pharmacol Ther 2013;37:411-9. [Crossref] [PubMed]
- Ciccarelli O, Lai Q, Goffette P, et al. Liver transplantation for hepatocellular cancer: UCL experience in 137 adult cirrhotic patients. Alpha-foetoprotein level and locoregional treatment as refined selection criteria. Transpl Int 2012;25:867-75. [Crossref] [PubMed]
- Robson R, Cecka JM, Opelz G, et al. Prospective registry-based observational cohort study of the long-term risk of malignancies in renal transplant patients treated with mycophenolate mofetil. Am J Transplant 2005;5:2954-60. [Crossref] [PubMed]
- Chong CR, Qian DZ, Pan F, et al. Identification of type 1 inosine monophosphate dehydrogenase as an antiangiogenic drug target. J Med Chem 2006;49:2677-80. [Crossref] [PubMed]
- Koehl GE, Wagner F, Stoeltzing O, et al. Mycophenolate mofetil inhibits tumor growth and angiogenesis in vitro but has variable antitumor effects in vivo, possibly related to bioavailability. Transplantation 2007;83:607-14. [Crossref] [PubMed]
- Benlloch S, Berenguer M, Prieto M, et al. De novo internal neoplasms after liver transplantation: increased risk and aggressive behavior in recent years? Am J Transplant 2004;4:596-604. [Crossref] [PubMed]
- Sgourakis G, Dedemadi G. Corticosteroid-free immunosuppression in liver transplantation: an evidence-based review. World J Gastroenterol 2014;20:10703-14. [Crossref] [PubMed]
- Goralczyk AD, Hauke N, Bari N, et al. Interleukin 2 receptor antagonists for liver transplant recipients: a systematic review and meta-analysis of controlled studies. Hepatology 2011;54:541-54. [Crossref] [PubMed]
- Wang XF, Li JD, Peng Y, et al. Interleukin-2 receptor antagonists in liver transplantation: a meta-analysis of randomized trials. Transplant Proc 2010;42:4567-72. [Crossref] [PubMed]
- Turner AP, Knechtle SJ. Induction immunosuppression in liver transplantation: a review. Transpl Int 2013;26:673-83. [Crossref] [PubMed]
- Kirk AD, Cherikh WS, Ring M, et al. Dissociation of depletional induction and posttransplant lymphoproliferative disease in kidney recipients treated with alemtuzumab. Am J Transplant 2007;7:2619-25. [Crossref] [PubMed]
- Fairfield C, Penninga L, Powell J, et al. Glucocorticosteroid-free versus glucocorticosteroid-containing immunosuppression for liver transplanted patients. Cochrane Database Syst Rev 2015;12:CD007606. [PubMed]
- Mazzaferro V, Llovet JM, Miceli R, et al. Predicting survival after liver transplantation in patients with hepatocellular carcinoma beyond the Milan criteria: a retrospective, exploratory analysis. Lancet Oncol 2009;10:35-43. [Crossref] [PubMed]
- Lee JH, Cho Y, Kim HY, et al. Serum tumor markers provide refined prognostication in selecting liver transplantation candidate for hepatocellular carcinoma patients beyond the milan criteria. Ann Surg 2016;263:842-50. [Crossref] [PubMed]
- Olson JC, Wiesner RH. Immunomodulating therapy in liver transplantation: principles and practice. Immunotherapy 2012;4:793-805. [Crossref] [PubMed]
- Lerut JP, Pinheiro RS, Lai Q, et al. Is minimal, [almost] steroid-free immunosuppression a safe approach in adult liver transplantation? Long-term outcome of a prospective, double blind, placebo-controlled, randomized, investigator-driven study. Ann Surg 2014;260:886-91. [Crossref] [PubMed]
- Krisl JC, Doan VP. Chemotherapy and transplantation: the role of immunosuppression in malignancy and a review of antineoplastic agents in solid organ transplant recipients. Am J Transplant 2017;17:1974-91. [Crossref] [PubMed]
- Selten J, Schlegel A, de Jonge J, et al. Hypo- and normothermic perfusion of the liver: Which way to go? Best Pract Res Clin Gastroenterol 2017;31:171-9. [Crossref] [PubMed]
- Li S, Yang F, Ren X. Immunotherapy for hepatocellular carcinoma. Drug Discov Ther 2015;9:363-71. [Crossref] [PubMed]
- Lai Q, Vitale A, Iesari S, et al. Intention-to-treat survival benefit of liver transplantation in patients with hepatocellular cancer. Hepatology 2017. [Epub ahead of print]. [Crossref] [PubMed]
Cite this article as: Lerut J, Iesari S, Foguenne M, Lai Q. Hepatocellular cancer and recurrence after liver transplantation: what about the impact of immunosuppression? Transl Gastroenterol Hepatol 2017;2:80.


