Modified palliative biliary stenting in situs inversus totalis patient with carcinoma gallbladder: feasibility and technical details
Introduction
Situs inversus (SI) is a congenital condition in which the major visceral organs are reversed or mirrored from their normal positions. Reported overall incidence of SI in adults is 1 in 5,000–20,000 (1). In the most common situation, SI totalis involves complete transposition (right to left reversal) of all of the abdominal organs. The exact anatomical relationship of the organs and the adjacent vasculature is essential prior to any complex hepatobiliary invasive procedures such as endoscopy, surgery and radiologic interventions in patients with SI. We report a case of successful percutaneous biliary stenting of carcinoma gallbladder in association with SI, with good clinical results.
Case presentation
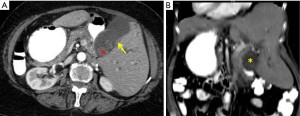
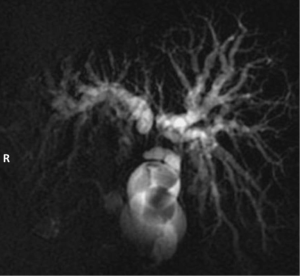
A 75-year-old female presented with one and a half months history of progressive painless jaundice, pruritus, and anorexia and weight loss. An incidental diagnosis of SI totalis was made on a prior abdominal sonography examination. On physical examination, a hard mass was palpated in the left hypochondrium. Abdominal sonography again demonstrated the SI, along with a left sided sub-hepatic mass with associated intrahepatic biliary radical dilatation (IHBRD). CT scan with contrast demonstrated a gallbladder mass causing hilar obstruction with resultant IHBRD (Figure 1). Magnetic resonance cholangiopancreatography (MRCP) showed abrupt biliary hilar obstruction consistent with malignant hilar biliary obstruction (Figure 2). Fine needle aspiration cytology confirmed the diagnosis of cholangiocarcinoma. Endoscopic retrograde cholangiopancreatography (ERCP) was unsuccessful, due to the variant anatomy. She was referred to interventional radiology for percutaneous biliary drainage and palliative biliary stenting.
Pre-procedural workup included platelet counts, coagulation profile [prothrombin time/international normalized ratio (PT/INR)], liver function tests as well as white count. Patient was kept fasting for 6 hours prior to the procedure and subcutaneous heparin dose was omitted. Subsequent to the pre-procedural workup, the patient was planned for percutaneous trans-hepatic biliary drainage, using fluoroscopic and ultrasound guidance. Few procedural modifications from the standard procedure protocol were made. The operator worked from the left side of the patient. This involved appropriate positioning of the monitors and ultrasound machine.
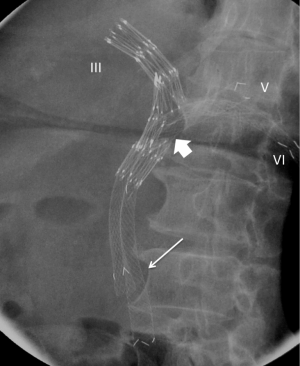
After obtaining informed written consent, the procedure was performed with fluoroscopic and ultrasound guidance and under all aseptic precautions. Conscious sedation using two rounds of 1 mg IV Midazolam and 50 µg of IV Fentanyl were performed under direct radiologist’s supervision. Sequential percutaneous punctures of segment III, V and VI biliary radicles were done, subsequently the hilar stricture was negotiated using a 0.035-inch 145-cm angled hydrophilic guidewire and was dilated using a 10 mm × 4 cm PTA angiography balloon (Cook, USA). Subsequently an indigenous stainless steel fenestrated biliary stent (HybridTM, patent awaited, Lucknow, India) was placed from the segment III puncture with fenestration at the hilum, facing segment V and VI (Figure 3). Then via the fenestration, 10 cm and 8 cm self-expendable kissing metallic stents (Niti-STM Taewong Medical, Seoul, Korea), were placed in segments VI and V respectively (Figure 3) with the distal end at the papilla. External biliary drainage catheters were then placed. Overall, total duration of the procedure exceeded by 25 minutes secondary to the complex anatomy. The total procedure time was approximately 65 minutes. Capping trial was started after 24 hours of the procedure.
Significant improvement in pruritus and liver functions were achieved. Follow up ultrasound examination showed resolution of previously identified IHBRD, with expected post procedural minimal residual pneumobilia. External catheters were removed on 4th post-procedural day after successful capping trial and the patient was discharged on the 5th post procedural day on injectable antibiotics for a total duration of ten days. Total hospital duration was 7 days including a post procedure hospital stay of 5 days.
Discussion
SI is a rare congenital anomaly, with reported incidence of 1 in 5,000–20,000 cases (1). It is hypothesized to be an autosomal recessive condition due to chromosomal abnormality, with a genetic locus on chromosome 12, leading to a reversal of left-right polarity of the organs (2). SI can be partial or total; simple or complicated.
A few case reports in literature document associations of SI with some benign and malignant diseases (3,4). Of note, a high incidence of pancreatic, bile duct and ampullary, hepatocellular and gastric cancers has been documented (5,6). SI concomitant with gallbladder cancer is a rare entity, with only one reported case (7). Several documented reports of surgical procedures in SI patients have encountered greater technical difficulties due to altered anatomy (8); however, the present case is the first report on the technical details and feasibility of percutaneous biliary interventions in this scenario.
Although literature is sparse on the technique modifications during surgery and endoscopy (5,8,9), there is none available on the details of technical alterations during radiologic interventions in SI cases. In the present case, special consideration was made regarding the right-left reversal and the complex biliary hilar anatomy. As the patient and the equipment was repositioned in the fashion that it simulates the normal anatomy instead of right-left reversal, it was observed during the procedure that the left handed interventionists don’t have an additional advantage.
The present case focuses on reconstruction of the malignant biliary hilar stricture using self-expandable metallic stents. We used the fenestrated stent in our patient to decrease the percutaneous access route and hence morbidity, similar to previously described cases (10). There are various technical advantages of extending the distal tip of the biliary stent across the ampulla. Firstly, two stents were deployed side by side in Y configuration so that one should not traverse the mesh of the other; secondly, were deployed simultaneously to maintain equal expansion rates and thirdly, it prevented the accidental over dilation at the ampulla and thus obviating the risk of ampullary injury.
In conclusion, the present case highlights the technical details as well as the modifications of a standard percutaneous biliary drainage procedure and biliary stenting in a case of gallbladder cancer in SI patient.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- Nursal TZ, Baykal A, Iret D, et al. Laparoscopic cholecystectomy in a patient with situs inversus totalis. J Laparoendosc Adv Surg Tech A 2001;11:239-41. [Crossref] [PubMed]
- Hummel KP, Chapman DB. Visceral inversion and associated anomalies in the mouse. J Heredity 1959;50:9-13.
- Macafee DA, Armstrong D, Hall RI, et al. Pancreaticoduodenectomy with a "twist": the challenges of pancreatic resection in the presence of situs inversus totalis and situs ambiguus. Eur J Surg Oncol 2007;33:524-7. [Crossref] [PubMed]
- Sato M, Watanabe Y, Iseki S, et al. Hepatolithiasis with situs inversus: first case report. Surgery 1996;119:598-600. [Crossref] [PubMed]
- Bilimoria MM, Parsons WG, Small W Jr, et al. Pancreaticoduodenectomy in a patient with ampullary carcinoma and situs inversus. Surgery 2001;130:521-4. [Crossref] [PubMed]
- Sceusi EL, Wray CJ. Pancreatic adenocarcinoma in a patient with situs inversus: a case report of this rare coincidence. World J Surg Oncol 2009;7:98. [Crossref] [PubMed]
- Shank PJ, Stafford RP. Complete situs viscerus inversus associated with cholelithiasis and complicated by carcinoma of the gallbladder. Rev Gastroenterol 1953;20:167-73. [PubMed]
- Kobus C, Targarona EM, Bendahan GE, et al. Laparoscopic surgery in situs inversus: a literature review and a report of laparoscopic sigmoidectomy for diverticulitis in situs inversus. Langenbecks Arch Surg 2004;389:396-9. [Crossref] [PubMed]
- Choi DH, Park JW, Kim BN, et al. Colonoscopy in situs inversus totalis patients. Am J Gastroenterol 2008;103:1311-2. [Crossref] [PubMed]
- Inal M, Akgül E, Aksungur E, et al. Percutaneous placement of biliary metallic stents in patients with malignant hilar obstruction: unilobar versus bilobar drainage. J Vasc Interv Radiol 2003;14:1409-16. [Crossref] [PubMed]
Cite this article as: Gupta N, Goyal P, Bansal I, Li S, Kumar Y, Baijal SS. Modified palliative biliary stenting in situs inversus totalis patient with carcinoma gallbladder: feasibility and technical details. Transl Gastroenterol Hepatol 2017;2:27.


