Type 2 gastric neuroendocrine tumor: report of one case
Case presentation
Medical history
The patient is a 47-year-old woman. The patient had suffered from upper abdominal pain, acid reflux, heartburn, nausea, and vomiting without any obvious cause since 2000. In 2005, gastroscopy in other hospital revealed “shimofuri” lesion with erosion in the duodental bulb, which was improved after omeprazole therapy. In 2009, gastroscopy in other hospital showed polyps in the greater curvature of stomach, which were treated with electrotomy (with unknown pathological findings). On April 1, 2014, abdominal ultrasound in other hospital revealed a solid mass sized about 3 cm × 2 cm in the head of pancreas. On April 2, 2014, somatostatin receptor scintigraphy showed high expression of somatostatin receptor in the tail and head of pancreas; the possibility of a neuroendocrine tumor (NET) was considered. Multiple high expressions of somatostatin receptor were also seen near the head of pancreas and in the retroperitoneal area; the possibility of lymph node metastasis could not be ruled out. High expression of somatostatin receptor was seen in right lobe of liver; the possibility of liver metastasis could not be ruled out. On May 4, 2014, biopsy of the space-occupying lesion in the head of pancreas showed the presence of tumor cells, which met the diagnostic criteria of an NET. On November 10, 2015, pathological consultation in our hospital showed that there was no mitotic figure; low-grade NET (G1) was considered. On May 27, 2014, targeted therapy was initiated in other hospital: oral administration with sutent 37.5 mg qd. Multiple abdominal/pelvic CT scans were performed, which showed the treatment response was “SD”.
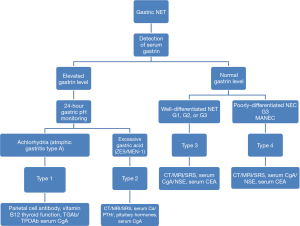
In January 2015, the patient for the first time visited our hospital due to “lower extremity edema and proteinuria” and began to receive traditional Chinese medicine (TCM)-based treatment. Laboratory tests showed: serum gastrin, 3,527 pg/mL (normal range, <100 pg/mL); serum CgA, 1,487.9 ng/mL (normal range, <100 ng/mL), CEA, 5.32 ng/mL; i-parathyroid hormone (PTH), 107.4 pg/mL; and blood calcium, normal. The thyroid function was normal, with both TPO-Ab and TG-Ab being negative. The patient’s general condition was fair. After daily oral administration of omeprazole the patient had no heartburn and acid reflux but suffered from fatigue, mild swelling of head and face, and backache. Urination and defecation were normal. On May 12, 2015, gastroscopy in our hospital (Figure 1) showed a polypoid uplift sized about 1.2 cm in the greater curvature of the middle part of stomach body. Biopsy showed: in gastric body: NET (G2); also, significant proliferation of gastric parietal cells was found in adjacent gastric mucosa. In gastric fundus: the proliferation of gastric parietal cells was obvious; immunohistochemistry showed the linear proliferation of neuroendocrine cells and hyperplasia of tiny nodules. In gastric antrum, the gastrin G cells showed linear hyperplasia. Immunohistochemistry: in gastric body: CK (AE1/AE3) (+), CgA (+), Syn (+), and Ki-67 (+10%). In gastric fundus: CgA (linearly and non-linearly + and tiny nodules +) and Syn (linearly and non-linearly + and tiny nodules +). In gastric autrum, gastrin (linearly +). Previous disease history: she developed diabetes 16 years ago and hyperlipidemia over 10 years ago. She underwent resection of pituitary tumor in 1998. In July 1, 2015, ultrasound found parathyroid hyperplasia. In 2002 and 2013, she received partial thyroidectomy, respectively, for thyroid tumors.
Case features
- The main symptoms in this patient were upper abdominal pain, heartburn, and acid reflux;
- Serum gastrin level remarkably elevated (3,527 pg/mL);
- On May 14, 2014, smear tests of the mass in the pancreatic head showed the presence of tumor cells, which met the diagnostic criteria of NET;
- On May 12, 2015 endoscopy showed a polypoid uplift (1.2 cm) in gastric body; pathology: NET (G2) in gastric body;
- Despite previous thyroid resection, parathyroid hyperplasia was detected by ultrasound in July 2015.
The current diagnoses included:
- Multiple endocrine neoplasia type 1 (MEN-1):
- Pancreatic NET (gastrinoma);
- Liver metastasis;
- Retroperitoneal lymph node metastasis;
- Type 2 gastric NET:
- Parathyroid hyperplasia after the surgery for pituitary tumor;
- Type 2 diabetes;
- Hyperlipidemia.
Treatment and follow-up results
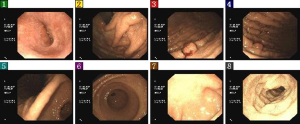
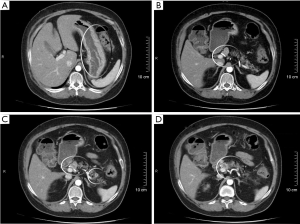
In May 2014, the patient began to use sutent 37.5 mg qd. In April 2, 2015, the dose of sutent was reduced to 25 mg qd due to side effects including high blood pressure and proteinuria. This drug was stopped on October 16, 2015. In January 2015, TCM drugs were added. On May 13, lanreotide (40 mg q14d) was added till today. On May 11, 2015, abdominal CT showed: (I) a nodule (0.8 cm) in pancreatic tail, and the possibility of a neoplastic lesion was considered; multiple nodules were seen on the upper part of the pancreatic head, and the possibility of swollen lymph nodes was considered; (II) thickening of the gastric wall. On May 11, 2015, abdominal contrast-enhanced CT in other hospital (Figure 2) showed that the treatment response was “SD”. On November 12, 2015, gastroscopy in our hospital (Figure 3) showed: The mucosa of the gastric body was slightly coarse, and three polyps sized 0.5–0.8 cm were seen in the upper and middle portions of the greater curvature of the stomach. Diagnosis: multiple polyps in the stomach. Biopsy showed: (polyps in gastric body) NET (G1), in which the mitotic figure was rarely seen and the Ki-67 about 1–2% +. Immunohistochemistry showed: in the gastric fundus, CgA (+), Syn (+), and Ki-67 (1–2%). Fundus of stomach: Mild chronic mucosal inflammation, lymphocyte accumulation, and linear proliferation of neuroendocrine cells. Immunohistochemical results: Ki-67 (1%), CgA (+), and Syn (+). On November 11, 2015, the findings of abdominal contrast-enhanced MRI were not remarkably different from those of abdominal contrast-enhanced CT on May 11, 2015. The treatment response was evaluated as “SD”.
Case summary
The patient had suffered from upper abdominal pain, acid reflux, heartburn since 2000.
In 2009, gastroscopy in other hospital showed polyps in the greater curvature of stomach, which were treated with electrotomy (with unknown pathological findings).
On April 2, 2014, somatostatin receptor scintigraphy showed high expression of somatostatin receptor in the tail and head of pancreas; the possibility of a NET was considered. The somatostatin receptor expression was also high near the head of the pancreas and in retroperitoneal lymph nodes and right lobe of liver; metastases were considered.
On May 4, 2014, biopsy of the space-occupying lesion in the head of pancreas showed that the findings met the diagnostic criteria of an NET, and the diagnoses included pancreatic NET, liver metastases, and retroperitoneal lymph node metastases.
On May 27, 2014 she began to receive targeted therapy: oral administration of sutent (37.5 mg qd).
From May 2014 to January 2015, she received regular examinations in other hospital, and the treatment response was evaluated as “SD”.
In January 2015, for the first time she visited our outpatient department and began to receive TCM treatment.
On April 2, 2015, the dose of sutent was lowered to 25 mg qd due to side effects.
On May 11, 2015, abdominal contrast-enhanced CT was performed, and the treatment response was evaluated as “SD”.
On May 12, 2015, gastroscopy in our hospital revealed a 1.2-cm polyp in gastric body; biopsy showed an NET (G2) in the gastric body.
On May 13, 2015, lanreotide (40 mg q14d) was added till today.
In August 2015, abdominal contrast-enhanced MRI in other hospital showed that the treatment response was "SD".
On October 16, 2015, the sutent treatment was stopped, and the treatment with lanreotide and TCM drugs continued.
On November 11, 2015, abdominal contrast-enhanced MRI was performed, and the treatment response was evaluated as “SD”.
On November 12, 2015, gastroscopy in our hospital revealed three polyps sized 0.5–0.8 cm in gastric body; biopsy showed NET (G1).
Discussion
Typing of gastric NETs
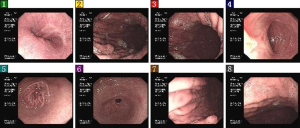
The well-differentiated gastric NETs can be divided into three types, which have different prognosis and treatment strategies. The typing algorithm of gastric NET is shown in Figure 4. In our current case, the pathology of the space-occupying lesion in pancreas confirmed the presence of an NET, with upper abdominal pain, acid reflux, and heartburn (Zollinger-Ellison syndrome) as the initial symptoms. Immunohistochemical findings included: serum gastrin, 3,527 pg/mL (normal range, <100 pg/mL) and serum CgA, 1487.9 ng/mL (normal range, <100 ng/mL). The diagnosis was pancreatic NET (gastrinoma). The previous histories included: In 1988, she underwent resection of pituitary tumors; on July 1, 2015, ultrasound detected parathyroid hyperplasia (i-PTH: 107.4 pg/mL). A diagnosis of multiple type 1 MEN was confirmed. Gastroscopy showed that there were multiple polyps in the gastric body and the mucous fold in gastric fundus and body were coarse and swollen. Puncture biopsy showed the presence of a G2 NET in gastric body. The diagnosis of a type 2 NET was confirmed.
Differentiation between type 2 and type 1 NETs
Type 1 gastric NET is associated with autoimmune atrophic gastritis, whereas type 2 was associated with gastrinoma/MEN-1. Both type 1 and type 2 can be associated with hypergastrinemia. The main difference is: type 1 patients often have achlorhydria, while type 2 patients have excessive gastric acid secretion. Thus, these two types can be differentiated by the typical symptoms and gastric acid monitoring result.
Type 2 gNET is relatively rare, accounting for about 5–6% of all gNETs. Its pathogenic mechanism is different from type 1. The hypergastrinemia in type 2 patients is related with gastrinoma/MEN-1; in fact, the gastrin is secreted by the tumor. Gastrinoma is often seen in the pancreas and the duodenum but is rarely found in gastric antrum and other sites. The pancreatic NET is often an MEN-1. The typical clinical manifestation of type 2 gastric NET is Zollinger-Ellison syndrome (i.e., heartburn and acid reflux) and may be associated with diarrhea, which may be alleviated after the use of PPI but may relapse after drug withdrawal. Serum gastrin level can remarkably increase (often higher than 1,000 pg/mL), along with excessive gastric acid secretion. The gastroscopic findings are similar between type 2 and type 1. The lesions are multiple and small in gastric fundus and gastric body, showing as polypoid uplifts; meanwhile the patients can also have hypertrophic gastritis or duodenal ulcer. Histopathology: most type 2 lesions are NET (G1) and NET (G2), along with parietal cell hyperplasia, which differs from the atrophic gastritis in type 1 patients, showing as hypertrophic gastritis.
Treatment of type 2 gNENs: the type 2 gNENs are mainly treated by the surgical resection of gastrinoma and its metastases. If the multiple metastases cannot be completely removed, somatostatin analogues may be applied. As the gastrin level drops, the polypoid lesions in the stomach may fade; meanwhile, PPI is often needed in type 2 patients for symptomatic treatment. The type 2 gNETs are often shown as multiple polypoid uplifts. Therefore, resection may be considered for tumors >1 cm; for tumors less than 1 cm, treatment of the primary lesions is more feasible.
Gastrinoma and MEN-1
Gastrinoma is a rare gastroenteropancreatic NET. It mainly arises from duodenum (75%) and pancreas (25%), and only very few of them (5%) arise from other organs such as stomach, liver, ovarian, and lung. It may cause Zollinger-Ellison syndrome, and the excessive secretion of gastrin can cause peptic ulcer disease and serious reflux esophagitis.
Pancreatic NETs (pNETs) can be either functioning or non-functioning. While most pNETs are non-functioning, the functioning pNETs include gastrinoma, insulinoma, glucagonoma, and vasoactive intestinal peptide tumor. A small group of pNETs (e.g., MEN-1 and von Hippel-Lindau’s syndrome) are the manifestation of hereditary NETs.
Clinically MEN-1 is mainly manifested as parathyroid adenoma, gastrointestinal and pancreatic tumors (mainly gastrinoma and insulinoma), and pituitary tumors (mainly prolactinoma). The most commonly invaded site is the parathyroid gland, followed by pancreatic and intestinal endocrine glands. MEN-1 is a hereditary tumor with high penetrance rate, with the mutation of MEN-1 tumor suppressor gene as its main pathogenetic mechanism. It may consist of more than 20 different combinations of endocrine or non-endocrine tumors, showing complex clinical symptoms. In particular, the gastrinoma tends to occur in duodenum, but may also be located in pancreas; it is often malignant and may already become metastatic at the time of diagnosis. Its typical manifestation is the Zollinger-Ellison syndrome.
The percentage of MEN-1 can reach 25% in gastrinoma patients. Thus, when a diagnosis of gastrinoma is made, the possibility of MEN-1 should be screened, during which the serum calcium, phosphorus and PTH, blood prolactin (PRL) and adrenocorticotropic hormone (ACTH), and plasma cortisol, norepinephrine, and epinephrine should be measured. Medical imaging techniques including cervical/abdominal ultrasound, abdominal contrast-enhanced CT/MRI, somatostatin receptor scintigraphy, and parathyroid ECT are helpful for locating the lesions.
Treatment of advanced pancreatic gastrinoma accompanied with type 2 gastric NET
In our current case, the patient had pancreatic gastrinoma with retroperitoneal lymph node metastases and liver metastases, which were also accompanied by type 2 gastric NET. Treatment of the primary lesion (gastrinoma) is essential. Surgical resection is preferred for resectable lesions; however, if the lesions cannot be surgically removed, medical treatment should be applied. The patient initially was treated with targeted therapy (sutent); however, due to severe side effects, its dose was reduced and finally the drug was stopped. Lanreotide +PPI+ TCM drugs were used instead, which achieved SD in the patient. Currently the patient’s general condition is fair, and the appetite and urination/defecation are normal. Gastroscopy has shown that the lesions inside the stomach are small (<1 cm) and do not require endoscopic treatment. The primary lesions (pancreatic and gastric gastrinoma) are still being treated.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Cite this article as: Li Y, Su X, Tan H. Type 2 gastric neuroendocrine tumor: report of one case. Transl Gastroenterol Hepatol 2016;1:88.