Metastatic multiple endocrine neoplasia type 1: report of one case
Case presentation
Disease history
A 46-year-old female patient was admitted due to “presence of space-occupying lesions in the liver for 2 months”. Health check-up showed no other special abnormalities. She had a history of hepatitis B for 6 years, during which she received antiviral therapy for 4 years but the drugs have been withdrawn for 2 years. In 2002, she underwent a surgery for a “pituitary tumor”, and its recurrence was treated with gamma knife radiosurgery. Follow-up showed no obvious abnormality.
On December 31, 2014, she suffered from abdominal discomfort associated with regurgitation and sought treatment in a local hospital, in which gastroscopy revealed “gastroduodenal ulcers”, along with elevated gastrin (>1,000.00 pg/mL). The symptoms were improved after antacid treatment.
On February 13, 2015, she visited Changhai Hospital, in which magnetic resonance imaging (MRI) showed multiple intrahepatic lesions; the possibility of neuroendocrine tumors (NETs) was considered.
On March 12, 2015, she sought treatment in Eastern Hepatobiliary Surgery Hospital, in which CT showed space-occupying lesions in the middle lobe of liver; malignancies (metastases?) were considered. The conditions might be space-occupying lesions between pancreas and stomach (lipoma?) or might be caused by pancreatic compression.
On March 12, 2015, she visited Changhai Hospital, in which PET-CT showed that nodules with increased metabolism at the junction between the descending and the horizontal sections of the duodenum; the possibilities of the gastrinoma with accompanying multiple hepatic metastases and the lipoma in the neck and body of the pancreas were considered.
On April 3, 2015, she visited the Fudan University Affiliated Tumor Hospital, in which liver biopsy showed NETs (G2), which were highly suspicous for metastatic diseases. Octreotide scan: suspicious for liver metastases of pancreatic NET.
On April 16, 2015, she sought treatment in our hospital and was suspicious for “pancreatic NET with hepatic metastases; space-occupying lesions in abdominal cavity; and lipoma”. She was then admitted.
Family history
Her eldest brother had a history of hepatitis (unknown type) with liver cancer and had died. Her second elder brother: had pituitary tumor and had undergone surgery; he had died of gastric cancer. Her third elder brother was healthy. The patient herself had pituitary tumor and had undergone surgery; she also had parathyroid adenoma, pancreatic NET with liver metastases, and abdominal lipoma. Her fifth younger brother had pituitary tumor and had undergone surgery; currently he is healthy. Her parents are healthy. Her husband and son are also healthy.
Physical examination
No positive sign was found.
Auxiliary examinations
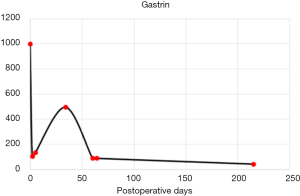
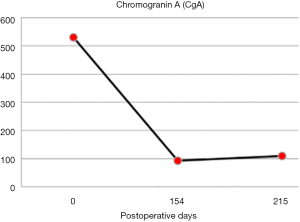
Auxiliary examinations performed on April 16, 2015 showed: liver function: total bilirubin, 4.5 µmol/L; direct bilirubin, 1.4 µmol/L; total protein, 64 g/L; albumin, 41 g/L; alanine aminotransferase, 33 U/L; aspartate aminotransferase, 31 U/L; prealbumin, 0.23 g/L; insulin-like growth factors, 32.8 ng/mL; insulin-like growth-factor-binding protein 3, 2.53 µg/mL; calcitonin, <2.00 pg/mL; growth hormone, 0.1 ng/mL; calcium, 2.67 mmol/L; parathyroid hormone (PTH), 135.1 pg/mL; adrenocorticotropic hormone, 39.5 pg/mL; cortisol, 111.4 nmol/L; angiotensin I, 0.40 µg/L; renin (active), 0.29 ng/mL/hr; angiotensin II, 46.25 pg/mL; prolactin, 902.2 mIU/L; hepatitis B virus surface antigen, (+) 6226COI; hepatitis B surface antibody, <2.0 mIU/mL; hepatitis B e antigen, (−) 0.096COI; hepatitis B e antibody, (+) 0.010COI; hepatitis B virus DNA, below detection limit; AFP, 2.3 ng/mL; CEA, 0.6 ng/mL; CA19-9, 9.1 U/mL; and NSE, 9.1 ng/mL. Chromogranin A (CgA), 530.32 ng/mL (normal range, <94 ng/mL). Gastrin: >1,000.00 pg/mL.
On April 16, 2015, gastroscopy revealed chronic gastritis (superficial) and space-occupying lesions at the junction between the duodental bulb and the descending part of duodenum. Biopsy: acute or chronic mucosal inflammation (at the junction between the duodental bulb and the descending part of duodenum).
On April 17, 2015, ultrasound showed space-occupying lesions with slightly low echoes in the right posterior lobe of liver, which was considered to be benign lesions; fatty infiltration of the liver and liver cysts were also found.
On April 17, 2015, upper abdominal MRI (plain + enhanced) indicated space-occupying lesions in the left medial lobe and right anterior lobe of the liver, which were considered to be metastatic lesions; lipoma in the gap between stomach and pancreas and nodules in left medial lobe of liver were also observed (Figure 1).
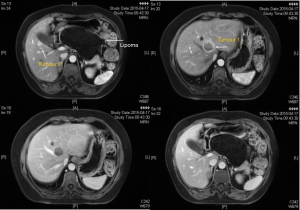
On April 24, 2015, pancreatic CT (plain + enhanced) revealed space-occupying lesions in left medial lobe and right anterior lobe of the liver, which were highly suspicious for metastases; lipoma in the peritoneal cavity was also considered, and well-differentiated liposarcoma was to be ruled out; nodules were found in the horizontal portion of the duodenum, and the possibility of MT was higher than duodenal papilla lesion; also, cysts in the left medial lobe of liver were also detected.
On April 30, pituitary MRI (plain + enhanced) revealed partially empty sella turcica; while the pituitary stalk was slightly thickened, no lesion with obviously abnormal signal was found inside the pituitary.
On April 30, 2015, parathyroid SPECT scans showed space-occupying lesions in right parathyroid area and abnormal concentrations of radioactivity, which were considered to be hyper-parathyroidism.
Based on the disease history, signs, and laboratory findings, the clinical diagnosis was metastatic multiple endocrine neoplasia type 1 (MEN1). Abdominal multiple lipomas also existed. After the surgery for pituitary tumor, organs involved by MEN1 included: pancreatic NET (gastrinoma) with liver metastasis; parathyroid adenoma; and pituitary tumor.
Diagnosis of MEN1
- Hyperparathyroidism √;
- Pituitary tumor √ (confirmed in a previous surgery);
- Pancreatic NET ?
Among which 2+/3 were met
- The possible accompanying conditions:
- Lung and thymus carcinoids;
- Adrenal tumor;
- Multiple lipomas √;
- Hemangiomas of the skin.
Among which 1/4 was met
Although the tumors were multiple and accompnaied with liver metastases, they were considered to be resectable after MDT consultation and thorough preoperative evaluation. According to the NCCN guidelines, multidisciplinary treatment in combination with surgery was planned.
Perioperative preparation
In the Department of Endocrine, various tests and endocrine axis assessment were completed; then, the levels of thyroxine and corticosteroids were adjusted to make the patient suitable for a surgery. In the Department of General Surgery, the surgical team carefully assessed the risk of pancreatic surgery, completed preoperative preparation, and then performed the resection of pancreatic tumor and liver metastases (in joint efforts with the Department of Liver Surgery). In the Department of Liver Surgery, the surgical team invited the Department of Endocrine to adjust the hormone levels and carried out surgery with the Department of General Surgery, with particular attention paid to postoperative endocrine hormone replacement and various stress conditions.
Surgical treatment
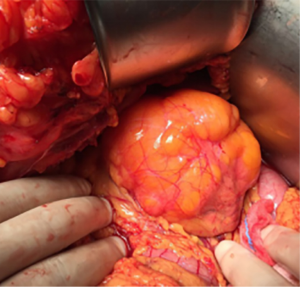
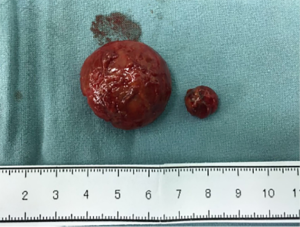
After active preoperative preparation, the patient underwent surgical treatment under general anesthesia on May 7, 2015. The intraoperative exploration had the following findings: pancreas: a tumor sized 1.5 cm was found on the surface of the tail of the pancreas; it was cherry-red in color, with clear borders and intact capsule (Figure 2). Duodenum: the duodenal bulb had moderate inflammation, in which scar-like tissue was touched; gastroscopy revealed chronic inflammation, which was considered to be inflammatory tissue. Lipoma: a retroperitoneal lipoma sized 12 cm × 9 cm × 9 cm was found above the head of the pancreas and behind the posterior wall of the stomach; it had clear borders and had no capsule (Figure 3). Liver: Two tumors (sized 3.5 cm and 1.5 cm, respectively) were found; they had clear borders, soft texture, and intact capsule (Figure 4). Surgery: In the Department of General Surgery, the pancreatic tumor and retroperitoneal lipoma were removed. In the Department of Liver Surgery, the liver metastases were removed. The surgery was smooth, and the intraoperative blood loss was 200 mL.
Post-operative pathology
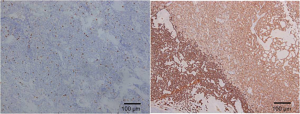
A NET at the tail of the pancreas, in which the cells were abundant, showed mild atypia. The mitotic figure was about 2/10 HPF. These findings met the diagnostic criteria of NET (G2). Immunohistochemistry (Figure 5): 15S13389-003, 4E-BP1 (partially +), ATRX (+), DAXX (+), Menin (absent), mTOR (+ on some membranes), P70S (partially +), PS6 (partially +), PTEN (+), somatostatin (−), TSC2 (+), SSR2 (++), SSR5 (part +), Syn (+), CHG (+), CD56 (focally +), wide-spectrum CK (partially +), gastrin (−), glucagon (partially +), insulin (−), Ki-67 (5% positive), P.P (partially +), and VIP (+).
An adipose tissue-derived tumor (pancreatic lipoma); the possibility of liposarcoma could not be ruled out due to its large size (maximum diameter: 15 cm) and tumor location. Genetic testing: dual-color fluorescence in situ hybridization (FISH2015-713): for CDK4, 50 tumor cells were counted, in which CEP12 value was 1–2 (mean: 1.8); the CDK4 gene was spotty, with a copy number of 1–2 (mean: 1.7). Thus, the FISH results were negative (CDK4 gene was not amplified). For CDK4, 50 tumor cells were counted, in which CEP12 value was 1–3 (mean: 1.9); the MDM2 gene was spotty, with a copy number of 1–3 (mean: 2.0). Thus, the FISH results were negative (MDM2 gene was not amplified).
Epithelioid cell tumors were found in liver; based on pathological findings and clinical history, metastatic NETs were considered.
According to the NCCN guidelines, adjuvant therapy with a long-acting somatostatin analogue (octreotide) was applied to prevent postoperative recurrence and metastasis. Sandostatin 30 mg was administered once monthly.
Regular follow-up visits were arranged for the patient.
On June 8, 2015, color Doppler ultrasound showed fatty infiltration of the liver and liver cysts. On July 9, 2015, color Doppler ultrasound showed suspected space-occupying lesions in right anterior lobe of liver (contrast-enhanced ultrasound was recommended), fatty liver, and hepatic cysts. On July 16, 2015, contrast-enhanced ultrasound showed solid lesion in right anterior lobe of liver (secondary MT was considered), fatty liver, and hepatic cysts.
On July 16, 2015, radiofrequency ablation of liver tumors was performed under local anesthesia.
On September 10, 2015, MRI did not find any recurrent lesion after liver MT surgery. On December 8, 2015, MRI did not find any recurrent lesion or post-RF treatment changes after liver MT surgery.
Blood gastrin and CgA levels were measured during long-term postoperative follow-up visits; currently they are within the normal levels (Figures 6,7).
Postoperative long-term follow-up showed that the fT3 and fT4 levels had remarkably decreased; on July 6, 2015, oral thyroxine tablets were used instead. Follow-up showed the decline in cortisol and corticosteroids levels; hydrocortisone was adjusted to the oral administration at a dosage of 25 mg in the morning and 12.5 mg at night. Follow-up showed that currently the prolactin level is normal. On July 6, 2015, the serum calcium was 2.9 mmol/L and the serum PTH level was 182.3 pg/mL. On December 8, 2015, the serum calcium was 2.81 mmol/L and the serum PTH level was 241.5 pg/mL.
The patient was admitted to the Department of General Surgery of our center on December 24, 2015 to treat the primary hyperthyroidism. Ultrasound at admission revealed a hypoechoic area on the dorsal side of the medial and upper portions of right thyroid lobe, which was considered to be a benign lesion arising from the parathyroid gland. Tests at admission showed the PTH was 203.4 pg/mL, the high-sensitivity thyroid hormone was 0.040 uIU/mL, and serum calcium was 2.65 mmol/L. Right parathyroidectomy was smoothly performed under general anesthesia on December 25, 2015. Postoperative pathology revealed epithelial hyperplasia in the parathyroid tissue. PTH was 148.1 pg/mL on the operative day.
Currently the patient is still under close follow-up.
Discussion
Surgical treatment of pancreatic neuroendocrine neoplasms (pNENs) with MEN1
The effectiveness of surgical treatmetn for gastrinoma, insulinoma, and non-functioning pNENs with accompanying MEN1 remains unclear. For insulinoma with accompanying MEN1, distal pancreatectomy (exenteration of tumor in pancreatic head) is recommended. For gastrinoma with accompanying MEN1, pancreaticoduodenectomy, routine multiple myeloma tumor resection and lymph node dissection are recommended. Cytoreductive surgery (>2.0 cm) is helpful to control symptoms (for insulinoma) and reduce the risk of metastasis (for gastrinoma).
As for metastatic pNETs, a potentially curative resection should be considered when a resection of complete or more than 90% of metastatic lesions along with the primary site could be achieved. Furthermore, a palliative surgery could be performed in selected functional pNETs because it may reduce tumor burden to alleviate hormonal syndrome and delay the subsequent need for therapy. Effective management of pNETs with liver metastases may mandate involvement of a team of specialists.
Acknowledgements
Funding: The study was funded by National Natural Science Foundation of China (Nos. 81401923, 81572294); CSCO-Novartis neuroendocrine tumor development fund (2013).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Cite this article as: Huang C, Zhu X, Han X, Lou W. Metastatic multiple endocrine neoplasia type 1: report of one case. Transl Gastroenterol Hepatol 2016;1:73.