Late recurrence of gastric cancer with isolated brain metastasis
Introduction
Brain metastasis from gastric cancer is rare and almost always accompanied by disseminated disease. We report an unusual case of a patient diagnosed with a sole metastatic lesion to the brain more than 4 years after presentation with locally advanced gastric adenocarcinoma, without extra-cranial disease.
Case presentation
JH presented in January of 2007 at the age of 70 with dysphagia and was found to have an ulcerating circumferential tumor of the gastroesophogeal junction that was confirmed a poorly differentiated adenocarcinoma. Imaging studies revealed non-metastatic disease. She received neoadjuvant chemotherapy with FOLFIRI (5FU/leucovorin/irinotecan) and underwent total gastrectomy in July 2007. Pathology showed an ypT2bN2M0 poorly differentiated adenocarcinoma extending into the subserosa and involving the proximal cardia and distal esophagus. Gallbladder, small bowel and the rest of the gastric pathology were negative for malignancy. The residual tumor was 3 cm × 3 cm × 1 cm in size with an R0 resection, the closest margin being 1.5 cm. Perineural and vascular invasion were present. Lymph node examination showed 4 of 27 nodes positive. Six cycles of adjuvant FOLFIRI chemotherapy were given and completed in November 2007. The patient was followed with regular surveillance first at her treating facility, Roswell Park Cancer Institute and subsequently at UCONN Health.
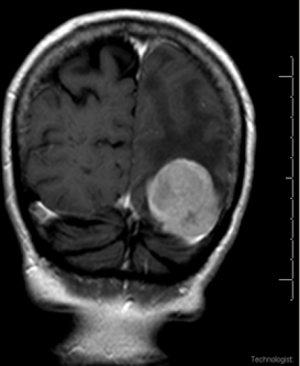
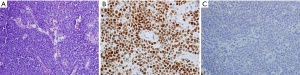
In early 2011 she began experiencing headaches, memory problems and word-finding difficulty. A neurological exam demonstrated right hemianopsia, nominal aphasia, recent and immediate memory problems, and an abnormal clock-drawing test. MRI of her brain in March 2011 showed a single 4.4 cm × 3.8 cm × 4.5 cm well-circumscribed lesion in the paramedian aspect of the left occipital lobe with surrounding vasogenic edema (Figure 1). Scans for other sites of metastatic disease were negative. The patient underwent stereotactic left parieto-occipital craniotomy with resection of the lesion. Pathology revealed a poorly differentiated adenocarcinoma comparable with her previous gastric cancer (Figure 2A,B). HER2 was not over-expressed (immunohistochemical 0/3) (Figure 2C).
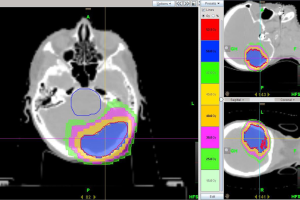
Post-operative radiation was administered using partial brain technique. A total of 50 Gy was delivered over 20 fractions using intensity modulated radiotherapy (IMRT) and image guided radiotherapy (IGRT) techniques with daily megavoltage CT on a Hi-Art Tomotherapy System® (Figure 3). The patient improved post-operatively, but developed several large nodular lesions on her scalp 1 month later. Biopsy of the scalp lesion and CSF analysis confirmed progressive metastatic involvement. She deteriorated rapidly and was transitioned to hospice.
Autopsy revealed metastatic poorly differentiated gastric carcinoma at the previous craniotomy site within the radiated field, also diffusely involving the leptomeninges, cerebellum and spinal cord, and focally involving the underlying brain parenchyma in the right parieto-occipital lobe, hippocampus, midbrain, cerebellum and pituitary gland. There was no evidence of malignancy in the bone, bone marrow, thorax, abdomen or pelvis or any site outside the brain.
Discussion
Gastric cancer remains a lethal malignancy both in the United States and globally. It is the 14th most common cancer in the United States with 24,590 new cases documented each year, resulting in more than 10,000 deaths annually (1). With 723,000 deaths worldwide, it is the third leading cause of cancer death for both sexes second only to lung cancer (2).
Brain metastasis is uncommon in gastric cancer; recurrence mostly occurs intra-abdominally. Extra-abdominal metastasis, usually involving lung and bone occurs in only about 13% of cases (3). A U.S. study that included over 3,000 gastric cancer cases over a 40-year period reported brain metastasis in only 0.7% of patients (4). In a study from Japan, 2,322 patients were identified to have gastric cancer from 1980 to 1998 and only 11 (0.47%) had metastatic brain lesions (5). Apart from these two large studies, the literature on gastric cancer metastatic to the brain consists mainly of case reports and limited case series.
In gastric cancer, brain metastasis occurring years after the initial diagnosis is rare and almost always accompanied by systemic relapse (4,5). A case series reported an interval period between diagnosis and development of brain metastasis ranging from 1 to 24 months (6). Our case is unique as the patient developed cerebral metastasis 4 years after initial diagnosis with no evidence of other systemic recurrent disease even at autopsy.
Our patient received perioperative chemotherapy for high grade gastric cancer, with a regimen utilized at the Roswell-Park Cancer Institute. She survived 4 years with no systemic recurrence only to relapse in brain with again high grade disease. HER2 positivity is found in 22% of gastric cancer cases (7). In breast cancer, it is associated with a higher incidence of brain metastasis (8), therefore looked for in our case, but negative.
The prognosis of gastric cancer patients who present with brain metastasis is dismal, and treatment is palliative. Response to treatment is poor in this cohort of patients (4,5). Treatment options include surgical resection (SR), brain radiotherapy, steroids, chemotherapy or a combination. The selection of treatment modality for these metastatic brain tumors depends on the number and resectability of the lesion(s) and the general health condition of the patient (9).
York et al. reported a median survival of 54 weeks (range, 22–83 weeks) in patients with gastric cancer with brain metastases who underwent SR, whole brain radiotherapy (WBRT) and steroid therapy (4). The median survival among the WBRT-alone group did not differ from patients who received steroid monotherapy (9.0 weeks with WBRT vs. 7.0 weeks with steroids, P>0.05). In retrospective analyses, the combination of SR and WBRT was associated with a survival advantage (4,10). A case series from Japan of four patients with cerebral gastric cancer metastases showed an overall survival ranging from 45–94 days post-treatment with SR and/or stereotactic radiosurgery (11). In solid tumors as a group, local brain radiotherapy (LBRT) following surgery was shown retrospectively to be similar to WBRT following surgery in patients with single brain metastasis in terms of local recurrence rate and median survival time (12). Because of this data, we treated our patient with LBRT in conjunction with SR, unfortunately with rapid tumor growth. The best approach to treatment of these patients remains unclear.
Our case illustrates that gastric cancer cells may lay dormant in the central nervous system for years and recur as virulent resistant disease. As combined modality treatments for initial therapy of aggressive cancers improve outcomes, cancer dormancy may become more apparent and recurrences seen in less common sites like brain. An understanding of cancer dormancy mechanisms and ways to target these small populations of cells is crucial to improving the outcome of these patients.
Acknowledgements
The authors appreciate the expertise of Poornima Hegde, MD for the choice and reproduction of pathology images.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient’s next of kin for publication of this manuscript and any accompanying images.
References
- American Cancer Society. Cancer facts and figures 2015. Atlanta: American Cancer Society, 2015.
- World Health Organization. Globocan 2012, estimated cancer incidence, mortality and prevalence worldwide in 2012. Available online: http://globocan.iarc.fr/Default.aspx
- Lee JL, Kang YK, Kim TW, et al. Leptomeningeal carcinomatosis in gastric cancer. J Neurooncol 2004;66:167-74. [Crossref] [PubMed]
- York JE, Stringer J, Ajani JA, et al. Gastric cancer and metastasis to the brain. Ann Surg Oncol 1999;6:771-6. [Crossref] [PubMed]
- Kasakura Y, Fujii M, Mochizuki F, et al. Clinicopathological study of brain metastasis in gastric cancer patients. Surg Today 2000;30:485-90. [Crossref] [PubMed]
- Kim M. Intracranial involvement by metastatic advanced gastric carcinoma. J Neurooncol 1999;43:59-62. [Crossref] [PubMed]
- Kang Y, Bang Y, Lordick F, et al. Incidence of gastric and gastro-esophageal cancer in the ToGA trial: correlation with HER2 positivity. American Society of Clinical Oncology Gastrointestinal Cancers Symposium; 2008 Jan 25-27; Orlando, FL, USA, abstr 11.
- Hicks DG, Short SM, Prescott NL, et al. Breast cancers with brain metastases are more likely to be estrogen receptor negative, express the basal cytokeratin CK5/6, and overexpress HER2 or EGFR. Am J Surg Pathol 2006;30:1097-104. [Crossref] [PubMed]
- Yamamoto M, Inagawa T, Kamiya K, et al. Twenty cases of metastatic brain tumor (in Japanese with English abstract). Shimanekenritsu Chuobyoin Igaku Zasshi 1987;14:62-6. (J Shimane Prefectural Central Hospital).
- Go PH, Klaassen Z, Meadows MC, et al. Gastrointestinal cancer and brain metastasis: a rare and ominous sign. Cancer 2011;117:3630-40. [Crossref] [PubMed]
- Tamura S, Takeno A, Miki H, et al. Clinical outcomes in patients with brain metastasis from gastric cancer. Gan To Kagaku Ryoho 2011;38:2093-6. [PubMed]
- Hashimoto K, Narita Y, Miyakita Y, et al. Comparison of clinical outcomes of surgery followed by local brain radiotherapy and surgery followed by whole brain radiotherapy in patients with single brain metastasis: single-center retrospective analysis. Int J Radiat Oncol Biol Phys 2011;81:e475-80. [Crossref] [PubMed]
Cite this article as: Philip AZ, Namakydoust A, Varilla VM, Macatangay C, Dowsett R, Tannenbaum SH. Late recurrence of gastric cancer with isolated brain metastasis. Transl Gastroenterol Hepatol 2016;1:61.


