Pediatric liver transplantation for hepatoblastoma
Hepatoblastoma is the most common pediatric liver tumor and is usually diagnosed before five years of age. It accounts for 1.2% of malignancies in patients less than 15 years of age (1). Recent studies report an increasing incidence of hepatoblastoma in the U.S. from 0.6 to 1.2 per million (2,3). Typically, patients present with an abdominal mass and elevated AFP. Increased risk for development of hepatoblastoma is associated with Beckwith-Wiedemann Syndrome, Familial Adenomatous Polyposis Coli, maternal tobacco exposure and very low birthweight (4-6). Treatment consists of a combination of chemotherapy and surgery, with the goal being attainment of complete local control by surgical resection and eradication of any extrahepatic disease.
Staging
By the surgery based Evans staging system, staging was based upon exploratory surgery at diagnosis for all patients. Stage I and II tumors are those resected at diagnosis with microscopically negative and positive margins, respectively. Stage III and IV tumors are unresectable at diagnosis without and with metastatic disease, respectively. The current COG protocol, AHEP0731, uses a risk stratification scheme that is a hybrid of the old Evans system and PRE-TEXT (Pretreatment Extent of disease) used to define the timing and extent of surgical resection (7). In PRE-TEXT, the tumor group (I, II, III, IV) defines the extent of hepatic parenchymal involvement and the PRE-TEXT annotation factors (V, P, E, F, R, C, N, M denoting hepatic veins or vena cava, portal vein, extrahepatic, multifocal, tumor rupture, caudate lobe, lymph node and metastatic disease, respectively) define unique tumor characteristics and the extent of extrahepatic disease. PRE-TEXT I and II tumors have 3 and 2 adjoining sections free of tumor, respectively, and are usually resectable at diagnosis or after neoadjuvant chemotherapy depending on vascular involvement. For PRE-TEXT III and IV tumors, only one or two nonadjoining sections or none, respectively, are free of tumor and major vessel involvement is common. When the vessels or all sections remain involved after chemotherapy the tumor may not be resectable. Recently, the Childhood Hepatic tumors International Collaboration (CHIC) was formed and developed a new risk stratification and staging system based on PRE-TEXT that will be the basis of the upcoming international liver tumors trial.
Resectability
Complete resection is a critical component for cure in the treatment of hepatoblastoma; however, 60% of tumors are unresectable at the time of diagnosis (8). Neoadjuvant chemotherapy is utilized and is often beneficial in rendering tumors resectable. Commonly, two adjuvant cycles of chemotherapy are reserved for administration post-operatively. Ortega et al. reported 20% of initially unresectable tumors remained unresectable after neoadjuvant chemotherapy. Otte et al. reported a need for liver transplantation for approximately 15% of patients with initially unresectable tumors (9).
Historical perspective: liver transplantation for hepatoblastoma
For patients whose tumors are too extensive to be conventionally resected, liver transplantation can be curative and has become an integral component of current treatment algorithms. In a recent study based on United Network for Organ Sharing (UNOS) registry data, the frequency of liver transplantation for hepatoblastoma increased from five in 1990 to 43 in 2013 (10). A review by Cruz et al. of the National Cancer Institute’s Surveillance, Epidemiology and End Results (SEER) registry [1975–2007], UNOS [1988–2010] and Children’s Hospital of Pittsburgh database [1987–2011] revealed a 20-fold increase in liver transplantation for hepatoblastoma over a 32-year period during which the frequency of hepatoblastoma cases increased 4-fold (11). The authors reported an increase in referral rate for liver transplantation for hepatoblastoma from 5% in early 1990s to 20% after 2004.
Indications for liver transplantation for hepatoblastoma
The Children’s Oncology Group (COG) recommends that only tumors where a segmentectomy or hemihepatectomy can be performed with a 1 cm tumor free margin on the middle hepatic vein and portal bifurcation be performed at diagnosis (1). Generally accepted indications for liver transplantation for hepatoblastoma include unifocal POST-TEXT IV (PRE-TEXT classification following chemotherapy) tumors and/or POST-TEXT III or IV with persistent widespread multifocality or major vessel involvement. Ideally, before a transplant there would be some response to chemotherapy. Depending on the surgeon, patients with POST-TEXT III tumors with major vascular involvement may be considered for an extreme conventional resection (conventional resection with major vascular reconstruction) instead of liver transplantation (7). In the nearly completed Childrens Oncology Group study AHEP0731, results are being analyzed for patients with POST-TEXT III with venous involvement and POST-TEXT IV tumors comparing conventional resection versus liver transplantation.
Contraindications to liver transplantation for hepatoblastoma
Transplant is contraindicated in the presence of any active regional or distant metastatic disease not cleared by chemotherapy or surgery (12,13). The treatment strategy for a patient who present with lung metastases with locally advanced tumors where liver transplantation is necessary to achieve tumor extirpation remain the most challenging subset population. Cruz et al. found that in their analysis of the Children’s Hospital of Philadelphia data, extrahepatic disease present prior to liver transplantation (but which had cleared by CT scan prior to transplant) was the main risk factor for recurrent hepatoblastoma post transplantation (11). Other analyses have found that risk of recurrence was similar for those who cleared with chemotherapy versus resection (10,14,15). Recommendations for bilateral lung palpation at the time of thoracotomy for persistent pulmonary disease following neoadjuvant chemotherapy remain controversial (1).
Liver transplantation in multifocal hepatoblastoma
Transplantation versus resection for patients with multifocal disease remains controversial with some recommending transplantation and others advocating for conventional resection when intrahepatic metastases clear with neoadjuvant chemotherapy (7,15-20). For patients with POST-TEXT IV multifocal tumors without metastatic disease after neoadjuvant chemotherapy, liver transplantation is clearly indicated (1).
Timing of liver transplantation
Prolonged chemotherapy administration attempting to render tumors resectable by conventional resection should be avoided. Several studies indicate that continuing to administer chemotherapy after four cycles does not increase the likelihood of conventional resectability of the tumor (21,22). In such patients, where liver transplantation is required to achieve local control, transplantation after four cycles of neoadjuvant chemotherapy is ideal (7).Unfortunately, this is not always possible due to unpredictable factors such as deceased organ donor availability. Héry et al. reviewed their experience with liver transplantation for hepatoblastoma and reported a wait time of 1–50 days for liver transplant (median 16 days); the authors concluded that delays in timing from last chemotherapy to transplant should be kept as short as possible (15). The concept of early referral for consultation (including consultation via telephone, email or other communication) for liver transplantation versus extreme liver resection was introduced by the current COG protocol AHEP0731 and the feasibility and outcome of this approach has been a major objective of that study. The goal is to decrease excessive toxicity due to prolonged chemotherapy and improve survival. In addition, Otte and others have shown that survival is higher (approximately 80% versus 30–40%) for patients who undergo primary liver transplantation (no attempt at conventional resection) as opposed to those in whom liver transplantation is utilized in the salvage setting (13,15,23-25).
Donor source
Utilization of living versus cadaveric donors for liver transplantation is dependent on the provider’s/institution’s approach. Benefits of living donor liver transplantation include control of the timing of transplantation resulting on potentially shorter wait times thereby eliminating dependence on cadaveric liver availability, but engender risk of a major operative procedure to a healthy donor (11,15). Benefits to cadaveric donor transplantation include longer blood vessels from cadaveric donor grafts that allow for easier vascular reconstruction (15). Interestingly, Pham et al. reported increased recurrence rate for those who waited longer on the liver transplantation list for a cadaveric donor liver (mean time of 31 versus 15 days for those with recurrence versus those without, respectively) (10).
Complications of liver transplantation
Peri- and post-operative complications following liver transplantation include primary nonfunction, hepatic artery and portal vein thrombosis, bleeding, bile leak, infection, acute cellular rejection, long term immunosuppressive medication complications, post transplant lymphoproliferative disease and chronic rejection (14). Cruz et al. reported an increased risk of hepatic artery thrombosis in patients with hepatoblastoma undergoing liver transplantation compared to those receiving liver transplants for other conditions (11); however, the PLUTO registry did not find any increase in incidence of this complication (26). Héry et al. reported no post-operative mortality in the month post transplant in 13 pediatric patients receiving liver transplantation for hepatoblastoma (15). Four patients experienced complications (bile leak in one patient, arterial thrombosis followed by re-transplantation in three patients). Of 30 patients undergoing liver transplantation for hepatoblastoma at a single institution, four patients developed hepatic artery and/or portal vein thrombosis with all four requiring retransplantation (10). Second malignancies were infrequently reported with one patient with Burkitt Lymphoma four years after surgery (15).
Survival following liver transplantation for hepatoblastoma
Survival results from different institutional reports of liver transplantation for hepatoblastoma are difficult to compare given the inability to compare by patient specifics such as PRE-TEXT/POST-TEXT grouping, chemotherapy regimens, age, comorbidities, timing of transplant from last chemotherapy, utilization of adjuvant chemotherapy post transplantation and status of metastatic disease at the time of transplant. Upon review of 292 patients (in 29 separate publications) with hepatoblastoma who underwent liver transplantation, 76% of patients were alive at the time of publication (Table 1 and Table S1). Of note, some manuscripts reviewed were not included when patients with hepatoblastoma were unable to be separately identified or when it was unclear if the patients had been previously reported. Of 41 patients (with details reported) with rescue liver transplantation after initial attempt at resection, seventeen were alive (41%) compared with 85% of 175 patients with primary liver transplantation. Post-transplant chemotherapy appeared to have been administered for 140 patients; however, it is difficult to assess any relation to outcome given that details were not reported for many patients and many confounding factors exist (for some patients, chemotherapy was given after transplantation for recurrent disease, whereas others did not include these specifics).

Full table
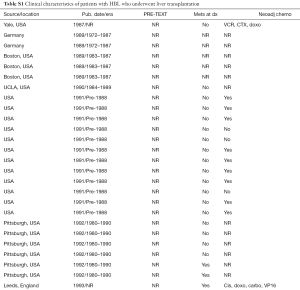
Full table
Conclusions
Liver transplantation can be curative in certain patients in whom conventional resection is not possible. Early consultation with pediatric liver transplantation specialists is critical in the management of patients with hepatoblastoma who are most likely to need liver transplantation or extreme liver resection and is important for facilitating timely resection by either conventional resection or liver transplantation (7). Though not without its complications (and lifelong immunosuppression), liver transplantation remains the treatment of choice for eligible patients otherwise incurable by conventional resection.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Pizzo PA, Poplack DG. Principles and Practice of Pediatric Oncology 7th ed. New York: Wolters Kluwer, 2016.
- Darbari A, Sabin KM, Shapiro CN, et al. Epidemiology of primary hepatic malignancies in U.S. children. Hepatology 2003;38:560-6. [Crossref] [PubMed]
- McLaughlin CC, Baptiste MS, Schymura MJ, et al. Maternal and infant birth characteristics and hepatoblastoma. Am J Epidemiol 2006;163:818-28. [Crossref] [PubMed]
- Trobaugh-Lotrario AD, Venkatramani R, Feusner JH. Hepatoblastoma in children with Beckwith-Wiedemann syndrome: does it warrant different treatment? J Pediatr Hematol Oncol 2014;36:369-73. [Crossref] [PubMed]
- Hirschman BA, Pollock BH, Tomlinson GE. The spectrum of APC mutations in children with hepatoblastoma from familial adenomatous polyposis kindreds. J Pediatr 2005;147:263-6. [Crossref] [PubMed]
- Spector LG, Feusner JH, Ross JA. Hepatoblastoma and low birth weight. Pediatr Blood Cancer 2004;43:706. [Crossref] [PubMed]
- Meyers RL, Tiao G, de Ville de Goyet J, et al. Hepatoblastoma state of the art: pre-treatment extent of disease, surgical resection guidelines and the role of liver transplantation. Curr Opin Pediatr 2014;26:29-36. [Crossref] [PubMed]
- Ortega JA, Douglass EC, Feusner JH, et al. Randomized comparison of cisplatin/vincristine/fluorouracil and cisplatin/continuous infusion doxorubicin for treatment of pediatric hepatoblastoma: A report from the Children's Cancer Group and the Pediatric Oncology Group. J Clin Oncol 2000;18:2665-75. [PubMed]
- Otte JB, de Ville de Goyet J, Reding R. Liver transplantation for hepatoblastoma: indications and contraindications in the modern era. Pediatr Transplant 2005;9:557-65. [Crossref] [PubMed]
- Pham TA, Gallo AM, Concepcion W, et al. Effect of Liver Transplant on Long-term Disease-Free Survival in Children With Hepatoblastoma and Hepatocellular Cancer. JAMA Surg 2015;150:1150-8. [Crossref] [PubMed]
- Cruz RJ Jr, Ranganathan S, Mazariegos G, et al. Analysis of national and single-center incidence and survival after liver transplantation for hepatoblastoma: new trends and future opportunities. Surgery 2013;153:150-9. [Crossref] [PubMed]
- Khaderi S, Guiteau J, Cotton RT, et al. Role of liver transplantation in the management of hepatoblastoma in the pediatric population. World J Transplant 2014;4:294-8. [Crossref] [PubMed]
- Otte JB. Paediatric liver transplantation--a review based on 20 years of personal experience. Transpl Int 2004;17:562-73. [PubMed]
- Meyers RL, Czauderna P, Otte JB. Surgical treatment of hepatoblastoma. Pediatr Blood Cancer 2012;59:800-8. [Crossref] [PubMed]
- Héry G, Franchi-Abella S, Habes D, et al. Initial liver transplantation for unresectable hepatoblastoma after chemotherapy. Pediatr Blood Cancer 2011;57:1270-5. [Crossref] [PubMed]
- Lautz TB, Ben-Ami T, Tantemsapya N, et al. Successful nontransplant resection of POST-TEXT III and IV hepatoblastoma. Cancer 2011;117:1976-83. [Crossref] [PubMed]
- International Childhood Liver Tumors Strategy Group (SIOPEL), Czauderna P, Otte JB, et al. Comments on surgical treatment of locally advanced hepatoblastoma. Cancer 2012;118:4092-3; author reply 4094-5. [Crossref] [PubMed]
- Baertschiger RM, Ozsahin H, Rougemont AL, et al. Cure of multifocal panhepatic hepatoblastoma: is liver transplantation always necessary? J Pediatr Surg 2010;45:1030-6. [Crossref] [PubMed]
- Dall'Igna P, Cecchetto G, Toffolutti T, et al. Multifocal hepatoblastoma: is there a place for partial hepatectomy? Med Pediatr Oncol 2003;40:113-6; discussion 116-7. [Crossref] [PubMed]
- Meyers RL, Tiao GM, Dunn SP, et al. Surgical management of children with locally advanced hepatoblastoma. Cancer 2012;118:4090-1; author reply 4094-5. [Crossref] [PubMed]
- von Schweinitz D, Hecker H, Harms D, et al. Complete resection before development of drug resistance is essential for survival from advanced hepatoblastoma--a report from the German Cooperative Pediatric Liver Tumor Study HB-89. J Pediatr Surg 1995;30:845-52. [Crossref] [PubMed]
- Warmann SW, Fuchs J. Drug resistance in hepatoblastoma. Curr Pharm Biotechnol 2007;8:93-7. [Crossref] [PubMed]
- Pimpalwar AP, Sharif K, Ramani P, et al. Strategy for hepatoblastoma management: Transplant versus nontransplant surgery. J Pediatr Surg 2002;37:240-5. [Crossref] [PubMed]
- Browne M, Sher D, Grant D, et al. Survival after liver transplantation for hepatoblastoma: a 2-center experience. J Pediatr Surg 2008;43:1973-81. [Crossref] [PubMed]
- Otte JB. Progress in the surgical treatment of malignant liver tumors in children. Cancer Treat Rev 2010;36:360-71. [Crossref] [PubMed]
- Otte JB, Meyers R. PLUTO first report. Pediatr Transplant 2010;14:830-5. [Crossref] [PubMed]
- Heimann A, White PF, Riely CA, et al. Hepatoblastoma presenting as isosexual precocity. The clinical importance of histologic and serologic parameters. J Clin Gastroenterol 1987;9:105-10. [Crossref] [PubMed]
- Ringe B, Wittekind C, Bechstein WO, et al. The role of liver transplantation in hepatobiliary malignancy. A retrospective analysis of 95 patients with particular regard to tumor stage and recurrence. Ann Surg 1989;209:88-98. [Crossref] [PubMed]
- Jenkins RL, Pinson CW, Stone MD. Experience with transplantation in the treatment of liver cancer. Cancer Chemother Pharmacol 1989;23 Suppl:S104-9. [Crossref] [PubMed]
- Olthoff KM, Millis JM, Rosove MH, et al. Is liver transplantation justified for the treatment of hepatic malignancies? Arch Surg 1990;125:1261-6; discussion 1266-8. [Crossref] [PubMed]
- Koneru B, Flye MW, Busuttil RW, et al. Liver transplantation for hepatoblastoma. The American experience. Ann Surg 1991;213:118-21. [Crossref] [PubMed]
- Tagge EP, Tagge DU, Reyes J, et al. Resection, including transplantation, for hepatoblastoma and hepatocellular carcinoma: impact on survival. J Pediatr Surg 1992;27:292-6; discussion 297. [Crossref] [PubMed]
- Lockwood L, Heney D, Giles GR, et al. Cisplatin-resistant metastatic hepatoblastoma: complete response to carboplatin, etoposide, and liver transplantation. Med Pediatr Oncol 1993;21:517-20. [Crossref] [PubMed]
- Superina R, Bilik R. Results of liver transplantation in children with unresectable liver tumors. J Pediatr Surg 1996;31:835-9. [Crossref] [PubMed]
- Bilik R, Superina R. Transplantation for unresectable liver tumors in children. Transplant Proc 1997;29:2834-5. [Crossref] [PubMed]
- Goss JA, Shackleton CR, McDiarmid SV, et al. Long-term results of pediatric liver transplantation: an analysis of 569 transplants. Ann Surg 1998;228:411-20. [Crossref] [PubMed]
- Al-Qabandi W, Jenkinson HC, Buckels JA, et al. Orthotopic liver transplantation for unresectable hepatoblastoma: a single center's experience. J Pediatr Surg 1999;34:1261-4. [Crossref] [PubMed]
- Dower NA, Smith LJ, Lees G, et al. Experience with aggressive therapy in three children with unresectable malignant liver tumors. Med Pediatr Oncol 2000;34:132-5. [Crossref] [PubMed]
- Srinivasan P, McCall J, Pritchard J, et al. Orthotopic liver transplantation for unresectable hepatoblastoma. Transplantation 2002;74:652-5. [Crossref] [PubMed]
- Molmenti EP, Wilkinson K, Molmenti H, et al. Treatment of unresectable hepatoblastoma with liver transplantation in the pediatric population. Am J Transplant 2002;2:535-8. [Crossref] [PubMed]
- Cillo U, Ciarleglio FA, Bassanello M, et al. Liver transplantation for the management of hepatoblastoma. Transplant Proc 2003;35:2983-5. [Crossref] [PubMed]
- Kasahara M, Ueda M, Haga H, et al. Living-donor liver transplantation for hepatoblastoma. Am J Transplant 2005;5:2229-35. [Crossref] [PubMed]
- Mejia A, Langnas AN, Shaw BW, et al. Living and deceased donor liver transplantation for unresectable hepatoblastoma at a single center. Clin Transplant 2005;19:721-5. [Crossref] [PubMed]
- Chen LE, Shepherd RW, Nadler ML, et al. Liver transplantation and chemotherapy in children with unresectable primary hepatic malignancies: development of a management algorithm. J Pediatr Gastroenterol Nutr 2006;43:487-93. [PubMed]
- Casas-Melley AT, Malatack J, Consolini D, et al. Successful liver transplant for unresectable hepatoblastoma. J Pediatr Surg 2007;42:184-7. [Crossref] [PubMed]
- Faraj W, Dar F, Marangoni G, et al. Liver transplantation for hepatoblastoma. Liver Transpl 2008;14:1614-9. [Crossref] [PubMed]
- Kosola S, Lauronen J, Sairanen H, et al. High survival rates after liver transplantation for hepatoblastoma and hepatocellular carcinoma. Pediatr Transplant 2010;14:646-50. [Crossref] [PubMed]
- Zsíros J, Maibach R, Shafford E, et al. Successful treatment of childhood high-risk hepatoblastoma with dose-intensive multiagent chemotherapy and surgery: final results of the SIOPEL-3HR study. J Clin Oncol 2010;28:2584-90. [Crossref] [PubMed]
- Kim T, Kim DY, Cho MJ, et al. Surgery for hepatoblastoma: from laparoscopic resection to liver transplantation. Hepatogastroenterology 2011;58:896-9. [PubMed]
- Ismail H, Broniszczak D, Kaliciński P, et al. Changing treatment and outcome of children with hepatoblastoma: analysis of a single center experience over the last 20 years. J Pediatr Surg 2012;47:1331-9. [Crossref] [PubMed]
- Kaliciński P, Ismail H, Broniszczak D, et al. Non-resectable hepatic tumors in children - role of liver transplantation. Ann Transplant 2008;13:37-41. [PubMed]
Cite this article as: Trobaugh-Lotrario AD, Meyers RL, Tiao GM, Feusner JH. Pediatric liver transplantation for hepatoblastoma. Transl Gastroenterol Hepatol 2016;1:44.


